Advanced Electrosurgical Bipolar Vessel Sealing to Control Intraoperative Bleeding in Hysterectomy: A Rapid Review and Meta-Analysis
DOI:
https://doi.org/10.14740/jcgo1553Keywords:
Hysterectomy, Bleeding, Electrosurgery, Vessel sealing, Rapid reviewAbstract
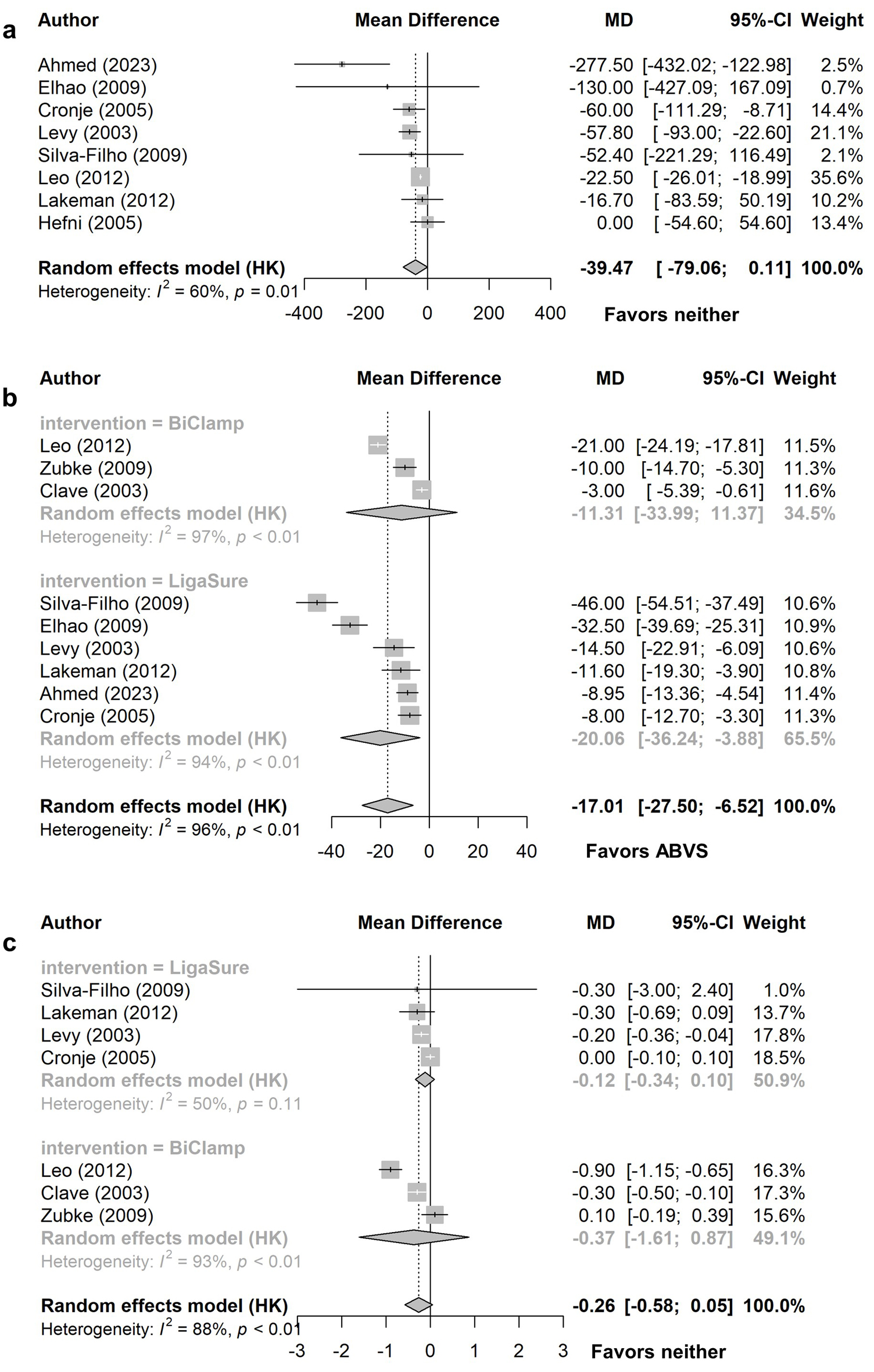
Background: Controlling intraoperative bleeding during hysterectomy is crucial and various methods exist to do this. Advanced electrosurgical bipolar vessel sealing (ABVS) may lead to improved outcomes compared to other hemostatic techniques. This rapid review aims to address the question “what is the clinical and cost effectiveness of ABVS compared with standard care for controlling intraoperative bleeding in hysterectomy?”
Methods: Medline, Embase, CINAHL, KSR Evidence, Cochrane Library, and the International Network of Agencies for Health Technology Assessment (INAHTA) HTA database were searched up to February 2025. Forward citation searching of included studies was conducted in Scopus. Systematic reviews and randomized controlled trials (RCTs) comparing ABVS to standard care for controlling intraoperative bleeding during abdominal, laparoscopic, or vaginal hysterectomies were included. Outcomes extracted included blood loss, operative time, complications, length of hospital stay, patient-reported pain, blood transfusions, health-related quality of life, resource use, and economic outcomes. Meta-analyses were conducted for each type of hysterectomy and pooled effect sizes were analyzed. Studies were synthesized narratively if not included in meta-analyses.
Results: One systematic review, one HTA, and 15 RCTs met the eligibility criteria. Meta-analyses found statistically significant differences in favor of ABVS over suturing for vaginal hysterectomy operative time and patient-reported pain the evening after surgery, abdominal hysterectomy blood loss and risk of requiring blood transfusion, and in favor of ABVS over conventional electrosurgical bipolar vessel sealing for total laparoscopic hysterectomy operative time. Two studies showed significantly lower blood loss with ABVS during subtotal laparoscopic hysterectomy. There were no statistically significant differences in other outcomes. A cost-consequence analysis from the UK perspective demonstrated high upfront costs associated with ABVS; however, potential cost savings were associated with reduced suture usage and lengths of hospital stay.
Conclusions: Use of ABVS during hysterectomy may lead to some improved outcomes compared to suturing or other energy devices; however, many outcomes are similar between methods. A lack of economic evidence means economic consequences are uncertain. Use of ABVS should be based on the type of hysterectomy performed, complexity of individual patients, and surgeons’ familiarity with devices.
Published
Issue
Section
License
Copyright (c) 2025 The authors

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.