Socioeconomic, Demographic, and Provider Determinants of Staged Versus Concomitant Surgery for Pelvic Organ Prolapse and Stress Urinary Incontinence
DOI:
https://doi.org/10.14740/jcgo1521Keywords:
Pelvic organ prolapse, Stress urinary incontinence, Mid-urethral sling, Staged surgery, Concomitant surgery, SociodemographicAbstract
Background: While concomitant surgery for pelvic organ prolapse (POP) and stress urinary incontinence (SUI) may benefit patients, variability exists in practice. A better understanding of the decision-making process regarding the placement of mid-urethral slings (MUSs) in women undergoing POP surgery is crucial for achieving equitable surgical planning and patient counselling. This study assessed factors associated with staged vs. concomitant SUI surgery in patients undergoing POP surgery.
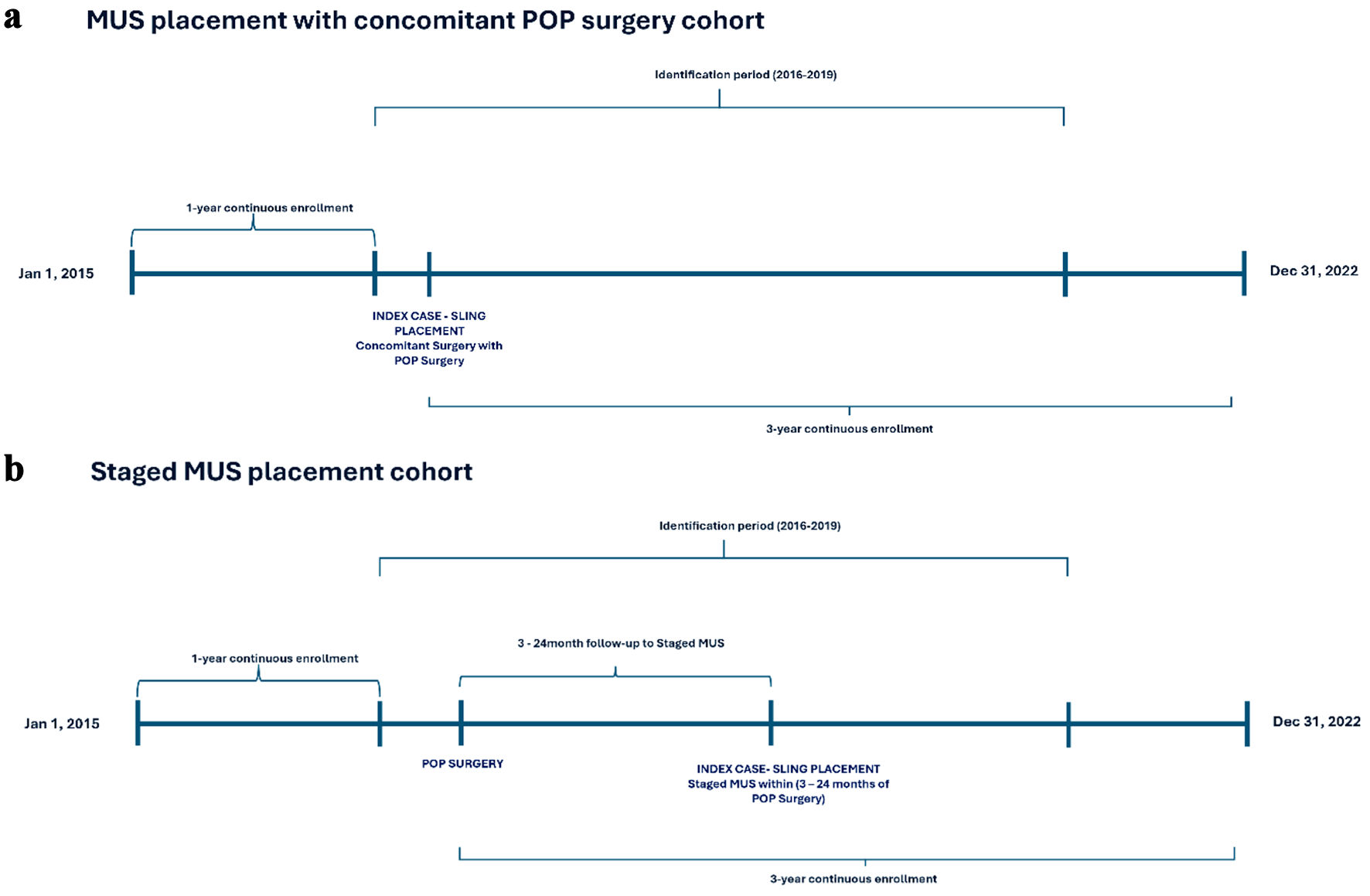
Methods: This retrospective cohort study used 100% Medicare Standard Analytical Files from 2016 to 2020. The sample population consisted of female patients surgically treated for POP with staged (within 24 months) or concomitant mid-urethral sling (MUS). Data were merged with the Agency for Healthcare Research and Quality (AHRQ) Social Determinants of Health Database. Multivariable logistic regression was used to assess independent associations between patient, location, and surgeon characteristics and the likelihood of staged versus concomitant procedures. Odds ratios (ORs) and 95% confidence intervals (CIs) were calculated.
Results: Among 40,842 patients with POP surgery, 96.7% (39,440) had concomitant, while 3.4% (1,402) had staged MUS. Most were aged 65 - 74 years (67.2%), Caucasian (91.7%), from urban areas (91.9%), and had Charlson Comorbidity Index ≤ 3 (82.3%). A higher likelihood of staged surgery was seen in White vs. other racial groups (example OR: 1.50 vs. Black, 95% CI: 1.03 - 2.18); in the South vs. other regions (example OR: 1.55 vs. Northeast, 95% CI: 1.26 - 1.91); and for obstetrics/gynecology vs. urologic surgeons (OR: 1.19, 95% CI: 1.02 - 1.40). Patients in counties with lower per capita income (OR: 1.02, 95% CI: 1.01 - 1.03), lower proportions of foreign-born (OR: 1.01, 95% CI: 1.01 - 1.05), limited English-speaking (OR: 1.03, 95% CI: 1.01 - 1.05), or uninsured (< 64 years of age; OR: 1.02, 95% CI: 1.00 - 1.03) households had higher likelihood of receiving staged surgery.
Conclusions: This study identified several demographic, socioeconomic, and surgeon-related factors associated with staged vs. concomitant MUS procedures among patients undergoing surgery for POP. The reasons for these differences are not fully understood and may reflect various underlying factors, including differences in communication, regional or specialty norms, patient choice, or other factors.
Published
Issue
Section
License
Copyright (c) 2025 The authors

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.