A Case of Mucous Membrane Pemphigoid Masquerading as Lichen Planus
DOI:
https://doi.org/10.14740/jcgo1545Keywords:
Mucous membrane pemphigoid, Vulvar pemphigoid, Vulvar lichen planus, Mucocutaneous diseaseAbstract
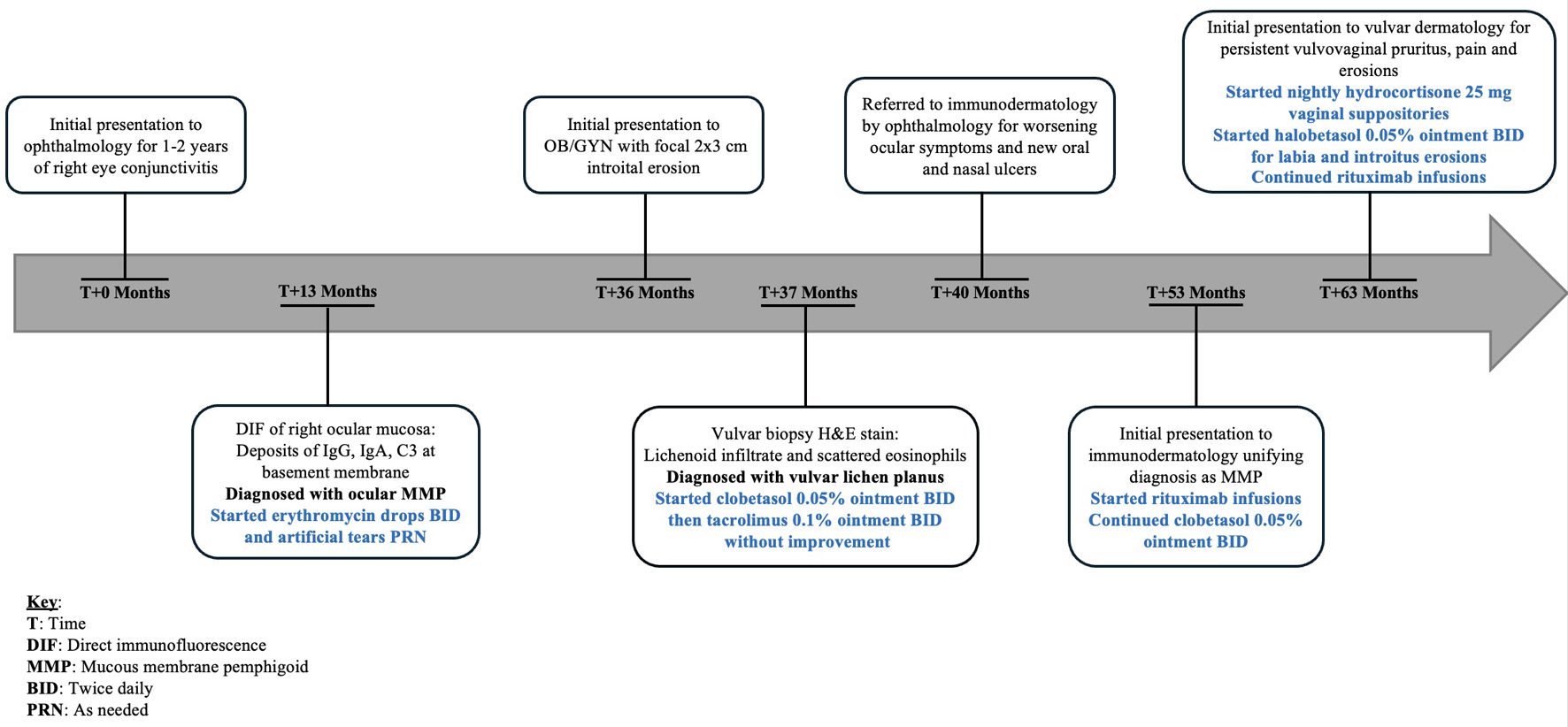
Mucous membrane pemphigoid (MMP) is a rare, autoimmune blistering disease that affects mucosal surfaces and can mimic other inflammatory dermatoses such as erosive lichen planus (LP), lichen sclerosus, and pemphigus vulgaris. Diagnosis is challenging due to overlapping clinical and histopathological features, especially when hematoxylin and eosin (H&E) staining reveals nonspecific lichenoid changes. We report the case of a 79-year-old woman with a 2-year history of therapy-resistant vulvar erosions, pruritus, and pain. Initial physical exam performed by gynecology noted a focal erosion of the introitus. A vulvar biopsy showed lichenoid infiltrate with scattered eosinophils. She was initially treated with clobetasol 0.05% ointment and tacrolimus 0.1% ointment for presumed LP, without clinical improvement. The patient had also developed erosions of the oral and nasal cavities, in addition to conjunctival injection and symblepharon, prompting a biopsy of the left conjunctiva by her ophthalmologist. Direct immunofluorescence (DIF) of the conjunctiva showed linear deposits of IgG, IgA, and C3 at the basement membrane zone, consistent with MMP. Upon referral to our vulvar dermatology clinic, she was receiving rituximab infusions for her MMP and applying clobetasol 0.05% ointment to her nasal, oral, and genital ulcers. Despite improvement in the nasal and oral ulcers, vulvovaginal pruritus and pain persisted. Exam in our office was notable for well demarcated pink patches on the bilateral medial labia majora with erosions beginning in the introitus and extending into the vagina with surrounding white hyperkeratotic epithelium. Architectural changes were seen including labial agglutination, partial clitoral phimosis, and introital stenosis. Given vaginal and introital involvement, she was started on nightly hydrocortisone 25 mg vaginal suppositories and halobetasol 0.05% ointment to be applied to the labia and introitus. At follow-up, the patient reported significant improvement in pain with minimal pruritus and notable improvement of the erosions and erythema. This case uniquely contributes to the literature by highlighting the diagnostic challenges of vulvar MMP and emphasizing the importance of maintaining a high clinical suspicion for MMP when lichenoid features are present on H&E, especially in the setting of extra-genital mucosal erosions. Early recognition and diagnostic confirmation with DIF are paramount for ensuring timely treatment initiation and prevention of irreversible disease progression.
Published
Issue
Section
License
Copyright (c) 2025 The authors

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.