| Journal of Clinical Gynecology and Obstetrics, ISSN 1927-1271 print, 1927-128X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Gynecol Obstet and Elmer Press Inc |
| Journal website https://jcgo.elmerpub.com |
Original Article
Volume 14, Number 4, December 2025, pages 167-175
Comparative Analysis of Intracervical Dinoprostone Gel and Vaginal Misoprostol for Labor Induction in a Primigravida at Term
Geeta Jamwala, Minakshi Ranaa, Raghu Naina Sharmaa, b
aGovernment Medical College Kathua, Jammu and Kashmir 184101, India
bCorresponding Author: Raghu Naina Sharma, Government Medical College Kathua, Jammu and Kashmir 184101, India
Manuscript submitted August 28, 2025, accepted October 31, 2025, published online December 11, 2025
Short title: PGE2 vs. Misoprostol for Labor Induction in Primiparas
doi: https://doi.org/10.14740/jcgo1539
| Abstract | ▴Top |
Background: The study addresses critical aspects of contemporary obstetric practices regarding labor induction in primigravida at term, focusing on the effectiveness and safety of intravaginal misoprostol (25 µg every 6 h for a maximum of four doses) and dinoprostone gel (0.5 mg every 6 h for a maximum of three doses).
Methods: It was a prospective interventional study. Inclusion criteria were: primigravida with an indication for labor induction, gestational age of 37 weeks or more, estimated fetal weight < 3.5 kg, Bishop score < 6 indicating an unfavorable cervix, singleton fetus, cephalic presentation, reactive fetal heart rate pattern, and patient consent. Exclusion criteria were: previous cesarean section uterine surgery, cephalo-pelvic disproportion, malpresentations, evidence of fetal distress pre-induction, grand multipara, fetal anomalies, intrauterine death, allergy to prostaglandins, major degree of placenta previa, and estimated fetal weight > 3.5 kg. Both the agents were compared in terms of: change in Bishop score (depending upon the doses of drugs and contractions), induction to active phase of labor, induction to delivery interval, total duration of labor, intrapartum complications (tachysystole, chorioamnionitis, rupture uterus), mode of delivery, fetal outcome at birth (fetal distress-hypoxia, bradycardia, meconium-stained liquor) Apgar score, postpartum complications like postpartum hemorrhage, and puerperal sepsis. Prospective interventional study was conducted among 200 primigravida women after meeting the strict inclusion and exclusion criteria of the hospital. Groups A and B were randomized with 100 patients each and maternal and fetal outcomes were studied. Partogram was used for monitoring and oxytocin was used as per necessity. Maternal and fetal outcomes were studied.
Results: The average gestational age was 38.74 ± 1.03 weeks, with a range of 37 to 41 weeks. The mean pre-induction Bishop score was 4.39 ± 1.02, with scores ranging from 2 to 6. The average total duration of labor experienced by these participants was 13.94 ± 4.43 h. The predominant indication for labor induction was identified as intrahepatic cholestasis of pregnancy (IHCP), accounting for 35.5% of cases. Subsequently, postdatism was the second most prevalent reason at 22.5%, followed by pregnancy-induced hypertension (PIH) at 19.5%. It was noted that the majority of pregnant women, approximately 90%, required only one to two doses of inducing agents, either intravaginal misoprostol or dinoprostone gel. While both agents were effective in initiating labor, intravaginal misoprostol demonstrated superiority in expediting labor progression and reducing the duration of labor. Both the agents exhibited comparable rates of neonatal and maternal complications, highlighting their overall safety and efficacy in clinical practice. In terms of the need for oxytocin in both groups, there was a statistically significant difference demonstrating better efficacy of misoprostol than dinoprostone gel.
Conclusions: While both intravaginal misoprostol and dinoprostone gel were successful in inducing labor, our results showed that intravaginal misoprostol was superior in several important areas.
Keywords: Intravaginal misoprostol; Intracervical dinoprostone; Labor induction; Primigravida
| Introduction | ▴Top |
The World Health Organization (WHO) defined normal labor in 1997 as “spontaneous in onset, low risk at the start, and remaining so throughout labor and delivery. This includes the spontaneous birth of an infant in vertex presentation between 37 to 42 completed weeks of gestation, with both mother and infant in good condition after delivery and no morbidity” [1].
Induction of labor is an obstetric procedure designed to artificially initiate the natural process of labor before spontaneous onset [2]. Indications for induction may include post-term pregnancy, pre-eclampsia, fetal growth restriction, premature rupture of membranes (PROM), or maternal medical conditions such as diabetes or hypertension. Conversely, contraindications to induction include placenta previa, umbilical cord prolapse, or previous uterine surgery such as classical cesarean section [2, 3]. Cervical ripening can be induced using a variety of methods which can be used in cases where the cervix is unfavorable prior to the start of the labor induction. Various techniques, such as the use of a balloon catheter, membrane sweeping, breast stimulation, sexual intercourse, ingestion of castor oil, a bath and/or enema, or acupressure and acupuncture are among the most commonly used methods to assist cervical ripening and induction of labor; each method has its own success rate.
Evening primrose oil (EPO) is one of the most common herbal preparations used by certified midwives across globe, to induce cervical ripening in pregnant women before the induction of labor. EPO is extracted from a yellow-flowering plant that grows wild in North America and parts of Europe and blooms in the evening. This oil is usually available in the form of soft gel and contains linoleic acid (70%) and gamma-linolenic acid (8-14%) [4]. Midwives are particularly interested in this plant because there is anecdotal evidence that the oil extracted from its seeds can soften the cervix, prevent post-term pregnancy, and shorten the duration of labor [5]. Previous studies on the efficacy of EPO on cervical ripening. Among the pharmacological agents commonly used for cervical ripening and induction of labor are misoprostol and dinoprostone (prostaglandin E2 (PGE2)). Misoprostol, a synthetic prostaglandin E1 (PGE1) analogue, is known for its efficacy in ripening the cervix and stimulating uterine contractions. It is administered orally, sublingually, or intravaginally. Dinoprostone, on the other hand, is a naturally occurring PGE2 analogue available as a gel or vaginal insert. It acts locally on the cervix to promote softening, effacement, and dilation [6].
Madaan et al in 2014 conducted a randomized trial on 100 pregnant women with term pregnancy, “Is low dose vaginal misoprostol better than dinoprostone gel for induction of labor: a randomized controlled trial” to compare the efficacy and safety profile of low dose vaginal misoprostol with dinoprostone gel for induction of labor in term pregnancies [7]. They also found that the vaginal misoprostol in low doses is similar in efficacy and safety to dinoprostone gel for cervical ripening and labor induction in term pregnancy.
De Bonrostro Torralba et al in 2018 conducted a prospective, randomized, open-labeled trial to compare the efficacy and safety of a low dose protocol of vaginal misoprostol and vaginal dinoprostone insert for induction of labor in women with post-term pregnancies [8]. They concluded that low-dose vaginal misoprostol and vaginal dinoprostone insert seem to be equally effective and safe for induction of labor in pregnant women with a gestational age beyond 41 weeks. Edward et al in 2001 conducted a systemic review and meta-analysis to compare dinoprostone 10 mg controlled-release vaginal insert with other forms of vaginal or cervical prostaglandin for cervical ripening. Randomized trials were included that compared a dinoprostone slow-release vaginal insert with an alternative vaginal or cervical prostaglandin for cervical ripening and labor induction in women at term with singleton gestations. Primary end points were delivery by 24 h post-insertion, uterine hypertonus with fetal heart change, and cesarean delivery rate [9].
By filling gaps in labor induction in term primigravida, this work could progress obstetrics. Comparisons were made in terms of Bishop score change (depending on drug doses and contractions), induction to active phase of labor, induction to delivery interval, total duration of labor, intrapartum complications (tachysystole, chorioamnionitis, rupture uterus), mode of delivery, fetal outcome at birth (fetal distress hypoxia, bradycardia, meconium-stained liquor), Apgar score, and postpartum complications.
| Materials and Methods | ▴Top |
This was a prospective interventional study conducted at the Department of Obstetrics and Gynaecology in Govt. Medical College and Associated Hospital, Kathua, over a 1-year duration from January 2023 to December 2023, after approval from the Hospital Ethical committee. Ethical clearance has been provided to this study by the institutional review board. All procedures performed in the study involving human participants were carried out following the institutional ethical standards. The study included 200 primigravida women meeting the inclusion criteria admitted to the labor ward of the associated hospital. Selection was randomized using computer-generated random numbers (random sequential allocation) as shown in Figure 1.
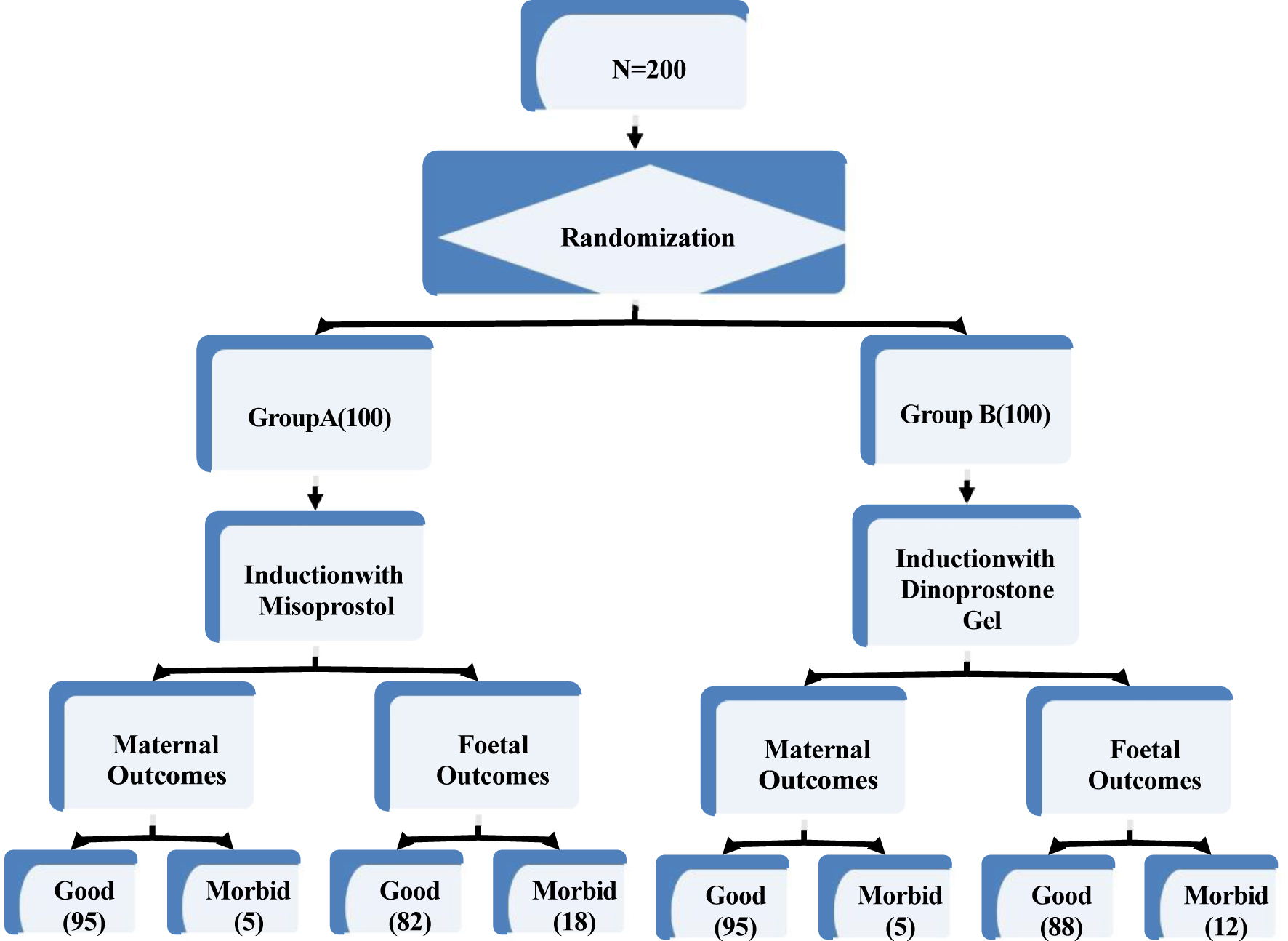 Click for large image | Figure 1. Flow chart of steps used in prospective interventional study with the maternal and fetal outcomes. |
Inclusion criteria
Inclusion criteria were: primigravida with an indication for labor induction, gestational age of 37 weeks or more, estimated fetal weight < 3.5 kg, Bishop score < 6 indicating an unfavorable cervix, singleton fetus, cephalic presentation, reactive fetal heart rate pattern, and patient consent.
Exclusion criteria
Exclusion criteria were: previous cesarean section or uterine surgery, cephalo-pelvic disproportion, malpresentations, evidence of fetal distress pre-induction, grand multipara, fetal anomalies, intra-uterine death, allergy to prostaglandins, major degree of placenta previa, and estimated fetal weight > 3.5 kg.
Group A consisted of 100 patients requiring induction who received 25 µg of intravaginal misoprostol, with a repeat dose given every 6 h for a maximum of four doses as necessary. Patients were examined at 6-h intervals to assess the improvement in the modified Bishop score. Observations were conducted according to the predetermined schedule, and oxytocin drip was initiated based on clinical requirements.
Group B consisted of 100 patients with an indication for induction who were administered 0.5 mg of intracervical dinoprostone gel, with a maximum of three doses repeated every 6 h as needed. Cases were reviewed 6 h after the first instillation to evaluate the modified Bishop score. If the score indicated poor progress, further instillations of dinoprostone gel were performed, and reassessment occurred every 6 h. Oxytocin drip was initiated based on clinical necessity. Labor progression was monitored using partogram in both groups once patients entered the active stage of labor. Continuous electronic monitoring of fetal heart rate and uterine contractions was available for each case.
Before initiating labor induction, Bishop score assessment and documentation were performed, and a normal fetal heart rate pattern was confirmed using electronic fetal monitoring.
Patients were reassessed after 6 h, oxytocin drip would be started as per requirement, progress would be monitored with the help of partogram in both the groups during the active stage of labor. Fetal heart rate monitoring will be done manually and with cardiotocography (CTG) machine. Women with failure of induction were taken for cesarean section. Both the groups would be compared on following outcomes.
Maternal outcome was measured in terms of change in Bishop score (depending upon the doses of drugs and contractions), induction to active phase of labor, time interval from induction to delivery, need for oxytocin augmentation, total duration of labor, mode of delivery (vaginal/lower segment cesarean section), intrapartum complications like meconium-stained liquor, uterine tachysystole/hypersystole, rupture uterus, failure of induction or non-progress of labor, and postpartum complications like postpartum hemorrhage and puerperia sepsis. Fetal outcome was noted in terms of fetal distress hypoxia (bradycardia), Apgar score at 5 min, and neonatal intensive care unit (NICU) admission rate.
The sample size was calculated using OpenEpi, version 3. Sample size was calculated taking α = 0.05 and β = 80%. Using formula based on estimated two means difference of 0.9 in improvement of Bishop score in previous studies, we found the sample size to be 100 in each of the two groups. A total of 200 cases were recruited, and each group consisted of 100 cases.
Data were compiled using Microsoft Excel and analyzed by IBM SPSS V.25. Descriptive statistics were computed to describe the sociodemographic characteristics of participants and to summarize the distribution of each of the dependent (outcome) and independent variables. Statistical tests, like Chi-square, Fisher’s, Levene t-test, etc. were considered significant when P-values are less than 0.05, and 95% confidence intervals (CIs) be presented throughout.
| Results | ▴Top |
In this study, a cohort of 200 primigravida women who qualified for the study as per inclusion and exclusion criteria were enrolled, with 100 participants assigned to receive intravaginal misoprostol and the remaining 100 assigned to receive dinoprostone gel, in accordance with the study protocol. The demographic characteristics of the study population indicated a mean age of 23.80 ± 3.4 years, ranging from 17 to 34 years. The average gestational age was 38.74 ± 1.03 weeks, with a range of 37 to 41 weeks. The mean preinduction Bishop score was 4.39 ± 1.02, with scores ranging from 2 to 6. The average total duration of labor experienced by these participants was 13.94 ± 4.43 h.
To mitigate potential selection bias associated with sequential allocation of patients, rigorous statistical analyses were conducted. Table 1 presents the results, which indicate no statistically significant differences between the two groups in terms of age, gestational age, Bishop score, and total duration of labor.
 Click to view | Table 1. Distribution of Baseline Pre-Induction Data of the Study Population |
In this investigation, the predominant indication for labor induction was identified as intrahepatic cholestasis of pregnancy (IHCP), accounting for 35.5% of cases. Subsequently, postdatism was the second most prevalent reason at 22.5%, followed by pregnancy-induced hypertension (PIH) at 19.5%.
It was noted that the majority of pregnant women, approximately 90%, required only one to two doses of inducing agents, either intravaginal misoprostol or dinoprostone gel. Furthermore, alterations in Bishop score were observed in 96.5% of the study cohort. Nonetheless, a need for oxytocin augmentation was identified in 81% of the pregnant participants under investigation. Following intervention, full-term vaginal delivery was achieved in 141 individuals (70.5%) within the study cohort, while the remaining patients underwent cesarean section for various obstetric indications.
It was noted that 85.0% of cases exhibited favorable fetal outcomes, while 15.0% experienced morbidity manifesting as respiratory distress, meconium aspiration syndrome (MAS), or a combination of both. Additionally, intrapartum complications in the form of tachysystole were observed in only two patients.
Postpartum complications were observed in 10 patients. Postpartum hemorrhage emerged to be having the highest frequency, which was followed by fever and wound sepsis.
The mean Apgar score at 1 min was determined to be 9.63 ± 0.88, with scores ranging from 6 to 10, and approximately 2.5% of newborns exhibited signs of respiratory depression after 1 min. Apgar scores at 5 min were found to be 9.92 ± 0.39, with scores ranging from 8 to 10.
A noteworthy observation was made regarding the change in Bishop score, with 99.0% of participants in the intravaginal misoprostol group experiencing alterations compared to 91.0% in the dinoprostone gel group. Statistical analysis revealed a significant difference with P value < 0.01, as demonstrated in Table 2. These findings suggest that intravaginal misoprostol exhibits superior efficacy in inducing labor compared to dinoprostone gel, as evidenced by its greater impact on Bishop score modification.
 Click to view | Table 2. Change in Bishop Score in Two Groups of Modes of Induction |
The statistical analysis indicated that this difference was not significant, with a P-value of 0.43, as depicted in Table 3. Therefore, while there is a numerical discrepancy in the rates of induction to the active phase of labor between the two groups, it does not reach statistical significance.
 Click to view | Table 3. Induction to Active Phase of Labor in Two Groups of Modes of Induction |
The study results indicated a statistically significant difference between the two groups in total duration of labor (h), induction to active phase of labor (h), and induction to delivery interval (h), with the intravaginal misoprostol group demonstrating superiority over the dinoprostone gel group, as shown in Table 4. Conversely, there was no statistically significant difference observed in the change of Apgar scores at 1 and 5 min between both groups.
 Click to view | Table 4. Comparison of Efficacy of Intravaginal Misoprostol and Dinoprostone Gel on Various Parameters of Induction of Labor and Apgar Score of Newborns |
Intravaginal misoprostol group showed efficacious induction to delivery interval group (h) as compared to dinoprostone gel group with statistically significant difference with P value < 0.01 as shown in Table 5.
 Click to view | Table 5. Induction to Delivery Interval Groups in Two Groups of Modes of Induction |
It was observed that there was a need for augmentation of labor with oxytocin in 95.0% of cases in dinoprostone gel group as compared to intravaginal misoprostol in which only 67.0% required same as shown in Table 6. This difference was statistically significant and substantiates the evidence for the better efficacy of intravaginal misoprostol in induction of labor.
 Click to view | Table 6. Need for Oxytocin Augmentation in Two Groups of Modes of Induction |
The outcome of full-term normal delivery was achieved in 71.0% of participants in intravaginal misoprostol group and 69.0% in dinoprostone gel group. However, the difference was not statistically significant (P = 0.87). The rate of cesarean sections was similar between the two groups (P = 0.87), indicating no association of cesarean section rates with the inducing agents used as shown in Table 7.
 Click to view | Table 7. Association of Cesarean Section Rates With the Inducing Agents in Two Groups |
In our study, we noted that two patients in the intravaginal misoprostol group experienced postpartum complications in the form of tachysystole. However, statistical analysis revealed that the difference in the incidence of tachysystole between the two groups was not statistically significant (P = 0.49) as shown in Table 8. This suggests that both intravaginal misoprostol and dinoprostone gel are equally safe for labor induction in terms of postpartum complications. No other complications such as chorioamnionitis or uterine rupture were observed in any of the women under study.
 Click to view | Table 8. Intrapartum Complications in Two Groups of Modes of Induction |
Similarly, no difference was found in postpartum complication in two groups under study as shown in Table 9.
 Click to view | Table 9. Postpartum Complications in Two Groups of Modes of Induction |
In our study, we observed that 18.0% of newborns in the intravaginal misoprostol group exhibited a morbid state, whereas only 12.0% of newborns in the dinoprostone gel group showed similar signs as shown in Table 10. However, statistical analysis revealed that the disparity in the incidence of newborn morbid states between the two groups was not statistically significant (P-value = 0.32). These findings suggest that there is no substantial difference in the occurrence of morbid states among newborns when labor induction is performed using intravaginal misoprostol compared to dinoprostone gel. Both agents appear to have similar safety profiles concerning newborn morbidity.
 Click to view | Table 10. Fetal Outcomes at Birth in Two Groups of Modes of Induction |
| Discussion | ▴Top |
The present study aimed to compare the efficacy and safety of intravaginal misoprostol versus dinoprostone gel for labor induction in primigravida women. The cohort comprised 200 primigravida participants, evenly divided between the two groups, with meticulous attention paid to inclusion and exclusion criteria. The demographic characteristics of the study population, including mean age, gestational age, and preinduction Bishop score, were comparable between the two groups, minimizing potential confounding factors.
This study reveals that IHCP, followed by postdatism and PIH, constituted the most prevalent reasons for induction in both study groups, accounting for 35.5%, 22.5%, and 19.5%, respectively. These results diverged from those of another study, where postdatism emerged as the primary cause, ranking second in our investigation. Plausible explanations for this disparity include the rising incidence of liver diseases, which may also affect pregnant women. Mikolasevic et al in 2018 disclosed that 3% of pregnant women experience some form of liver disease during pregnancy, potentially contributing to IHCP [10]. Additionally, Prajer et al noted a predominance of inductions due to postmaturity in their study, further corroborating our findings [11].
Furthermore, our study demonstrated that the mean total duration of labor was shorter in the misoprostol group (12.38 ± 4.55 h, P-value < 0.05). The induction to active phase of labor (6.16 ± 4.55 h, P-value < 0.05), and induction to delivery interval (10.84 ± 4.40 h, P-value < 0.05) were also reduced in the intravaginal misoprostol group, indicating its superiority over dinoprostone gel, as depicted in Table 4. These findings were consistent with studies pursuing similar objectives. Ayad in 2202 demonstrated that the use of misoprostol was linked to quicker delivery and reduced need for oxytocin [12]. Conversely, Chaudhuri et al in 2011 reported that vaginal misoprostol may offer efficacy comparable to PGE gel for labor induction after PROM at term [13].
Our investigation indicates that both intravaginal misoprostol and dinoprostone gel were effective in inducing labor, as demonstrated by significant alterations in Bishop score observed in the majority of participants in both groups after 6 h of intervention. However, the intravaginal misoprostol group exhibited superior efficacy (P-value < 0.01), suggesting a more pronounced effect on cervical ripening and labor progression compared to dinoprostone gel. This finding aligns with research from India, which also found a significant difference in post-induction mean Bishop score when PGE1 was administered vaginally [14]. Moreover, a significantly lower proportion of patients in the intravaginal misoprostol group required augmentation of labor with oxytocin (67.0% vs. 95.0%), consistent with evidence from Pakistan comparing oral PGE1 with intracervical PGE2 [15] and Jha et al [16].
Although the rates of induction to the active phase of labor were numerically higher in the intravaginal misoprostol group, this disparity did not attain statistical significance, indicating comparable efficacy between the two agents in this aspect. Nevertheless, notable disparities were evident in the total duration of labor, induction to active phase of labor, and induction to delivery interval, with the intravaginal misoprostol group demonstrating superiority over the dinoprostone gel group. These findings imply that intravaginal misoprostol may offer advantages in terms of expediting labor progression and reducing the overall duration of labor compared to dinoprostone gel.
An appreciable improvement in Bishop score at 6 h was noted in the misoprostol group after using one to two doses in more than 90.0% of cases, as illustrated in Table 2. This outcome is consistent with previous studies. For instance, Sanchez-Ramos et al in 1993, in their study comparing misoprostol 50 mg intravaginally every 4 h with oxytocin, demonstrated a significant improvement in the score [17]. Similarly, Wing et al in 1995, in their study comparing 50 mg of intravaginal misoprostol every 3 h with 0.5 mg of intracervical dinoprostone every 6, also reported an enhancement in score at 3 h of intervention [18]. Buser et al (1997), in their study utilizing 50 mg of intravaginal misoprostol and 0.5 mg intracervical cerviprime, also observed an improvement in the score, consistent with our study results [19].
Despite variations in labor outcomes, our analysis revealed no significant differences in neonatal well-being between the two groups. Apgar scores at 1 and 5 min were notably high in both cohorts, indicating overall good neonatal health. Furthermore, the incidence of neonatal respiratory depression was minimal and comparable between the groups, further affirming the safety profile of both labor induction agents. These findings are consistent with prior research [12, 13] and are in alignment with those of the EXPEDITE study [20]. Neonatal outcomes in our investigation did not show statistical significance and were similar to those reported by Ayad [12] and Chaudhuri et al [13].
Regarding maternal outcomes, our study identified a comparable rate of full-term normal deliveries and cesarean sections between the two groups, indicating no association of cesarean section rates with the inducing agents used. Similarly, the incidence of postpartum complications, including tachysystole and morbid states among newborns, did not significantly differ between the groups, suggesting comparable safety profiles for both intravaginal misoprostol and dinoprostone gel in this context. Although an increased risk of tachysystole is an anticipated outcome when using misoprostol, as demonstrated in several studies [21-23].
A notable finding was the statistically significant difference in Bishop score modifications between the two groups, with a higher proportion of participants in the intravaginal misoprostol group experiencing alterations compared to the dinoprostone gel group. However, the findings of this study should be interpreted with caution, as different hospitals may follow varying protocols for labor induction, which could influence outcomes. Therefore, the results may not be directly generalizable to other settings.
Conclusion
Our study aimed to compare the efficacy and safety of intravaginal misoprostol versus dinoprostone gel for labor induction in primigravida women. We meticulously designed our cohort, comprising 200 primigravida participants evenly divided between the two groups, ensuring comparability in demographic characteristics and minimizing potential confounding factors. Our findings indicate that while both intravaginal misoprostol and dinoprostone gel were effective in inducing labor, intravaginal misoprostol demonstrated superiority in several key aspects.
Firstly, we observed that the most common indications for induction in both groups were IHCP followed by postdatism and PIH. This finding diverged from previous studies, possibly indicating an emerging trend related to liver diseases affecting pregnant women. Additionally, we found that the mean total duration of labor, induction to active phase of labor, and induction to delivery interval were significantly shorter in the intravaginal misoprostol group compared to the dinoprostone gel group, consistent with prior research. As this was not a double-blind study, both participants and outcome assessors were aware of the intervention, which may have introduced observer or performance bias, especially in subjective assessments such as changes in the Bishop score.
Our study also revealed a higher proportion of participants in the intravaginal misoprostol group experiencing significant alterations in Bishop score compared to the dinoprostone gel group after 6 h of intervention. This suggests that intravaginal misoprostol may exert a more pronounced effect on cervical ripening and labor progression. Importantly, neonatal well-being did not significantly differ between the two groups, with reassuringly high Apgar scores at 1 and 5 min and comparable rates of neonatal respiratory depression. Neonatal outcomes in this study were restricted to Apgar scores and short-term morbid conditions observed during the immediate post-delivery period. Long-term neonatal follow-up was not performed, which limits assessment of sustained safety outcomes.
Maternal outcomes, including rates of full-term normal deliveries and cesarean sections, also did not significantly differ between the two groups, indicating comparable safety profiles.
However, it is worth noting that intravaginal misoprostol was associated with a higher risk of tachysystole, as expected with its use, although this did not translate into adverse neonatal outcomes in our study. The relatively small sample size may limit the ability to detect rare but serious maternal or neonatal adverse events, including uterine rupture and severe neonatal complications. The study was not powered to capture such infrequent outcomes. Another thing that we would like to highlight is, although oxytocin augmentation was carried out as per institutional protocol, minor variations in clinical judgement and practitioner practice could have influenced induction and labor outcomes.
Acknowledgments
The authors are thankful to the Principal GMC Kathua for permission to carry out this study. We also thank the staff of Department of Obstetrics and Gynecology, GMC Kathua for their cooperation and help during the study.
Financial Disclosure
The authors have received no funding from any agencies to conduct this study.
Conflict of Interest
The authors declare no conflict of interest.
Informed Consent
Not applicable.
Author Contributions
Geeta Jamwal: writing original draft and clinical study; Minakshi Rana: supervision, writing, review, and editing; Raghu Naina Sharma: writing, review, editing, and clinical study.
Data Availability
Any inquiries regarding supporting data availability of this study should be directed to the corresponding author.
| References | ▴Top |
- Arulkumaran S, Penna LK, Bhasker Rao K. Chapter 1. Physio-pharmacology of labour; Chapter 18. Induction of labour. The management of labour. 2nd ed. 2004
- Satoskar RS, Bhandarkar SD, Rege NN. Pharmacology and pharmacotherapeutics. 25th ed. Antifertility agents and ovulation-inducing drugs. Ch-66, p. 956.
- Guyton AC, Hall JE. Unit-14, Ch-81. Female physiology and female hormones. Textbook of medical physiology. 11th ed. p. 1016-1019.
- Lee MR. The history of ergot of rye (Claviceps purpurea) II: 1900-1940. J R Coll Physicians Edinb. 2009;39(4):365-369.
doi pubmed - Moir J. Induction of premature labour. Trans Edinb Obstet Soc. 1898;23:15-33.
pubmed - Gibbs RS, Karlan BY, Haney AF, Nygaard I. Danforth's obstetrics and gynecology. 10th ed. Ch.11. Preterm labour and post-term deliveries. p. 167.
- Madaan M, Agrawal S, Puri M, Nigam A, Kaur H, Trivedi SS. Is low dose vaginal misoprostol better than dinoprostone gel for induction of labor: a randomized controlled trial. J Clin Diagn Res. 2014;8(9):OC31-34.
doi pubmed - De Bonrostro Torralba C, Tejero Cabrejas EL, Envid Lazaro BM, Franco Royo MJ, Roca Arquillue M, Campillos Maza JM. Low-dose vaginal misoprostol vs vaginal dinoprostone insert for induction of labor beyond 41st week: A randomized trial. Acta Obstet Gynecol Scand. 2019;98(7):913-919.
doi pubmed - Hughes EG, Kelly AJ, Kavanagh J. Dinoprostone vaginal insert for cervical ripening and labor induction: a meta-analysis. Obstet Gynecol. 2001;97(5 Pt 2):847-855.
doi pubmed - Mikolasevic I, Filipec-Kanizaj T, Jakopcic I, Majurec I, Brncic-Fischer A, Sobocan N, Hrstic I, et al. Liver Disease During Pregnancy: A Challenging Clinical Issue. Med Sci Monit. 2018;24:4080-4090.
doi pubmed - Prager M, Eneroth-Grimfors E, Edlund M, Marions L. A randomised controlled trial of intravaginal dinoprostone, intravaginal misoprostol and transcervical balloon catheter for labour induction. BJOG. 2008;115(11):1443-1450.
doi pubmed - Ayad IA. Vaginal misoprostol in managing premature rupture of membranes. East Mediterr Health J. 2002;8(4-5):515-520.
pubmed - Chaudhuri S, Mitra SN, Banerjee PK, Biswas PK, Bhattacharyya S. Comparison of vaginal misoprostol tablets and prostaglandin E2 gel for the induction of labor in premature rupture of membranes at term: a randomized comparative trial. J Obstet Gynaecol Res. 2011;37(11):1564-1571.
doi pubmed - Mahendru R, Yadav S. Shortening the induction delivery interval with prostaglandins: a randomized controlled trial of solo or in combination. J Turk Ger Gynecol Assoc. 2011;12(2):80-85.
doi pubmed - Munzar Z. A comparison of oral misoprostol and vaginal prostaglandin E2 tablets for induction of labour at term. Pak Armed Forces Med J. 2015;65(3):301.
- Jha N, Sagili H, Jayalakshmi D, Lakshminarayanan S. Comparison of efficacy and safety of sublingual misoprostol with intracervical dinoprostone gel for cervical ripening in prelabour rupture of membranes after 34 weeks of gestation. Arch Gynecol Obstet. 2015;291(1):39-44.
doi pubmed - Sanchez-Ramos L, Kaunitz AM, Del Valle GO, Delke I, Schroeder PA, Briones DK. Labor induction with the prostaglandin E1 methyl analogue misoprostol versus oxytocin: a randomized trial. Obstet Gynecol. 1993;81(3):332-336.
pubmed - Wing DA, Jones MM, Rahall A, Goodwin TM, Paul RH. A comparison of misoprostol and prostaglandin E2 gel for preinduction cervical ripening and labor induction. Am J Obstet Gynecol. 1995;172(6):1804-1810.
doi pubmed - Buser D, Mora G, Arias F. A randomized comparison between misoprostol and dinoprostone for cervical ripening and labor induction in patients with unfavorable cervices. Obstet Gynecol. 1997;89(4):581-585.
doi pubmed - Wing DA, Brown R, Plante LA, Miller H, Rugarn O, Powers BL. Misoprostol vaginal insert and time to vaginal delivery: a randomized controlled trial. Obstet Gynecol. 2013;122(2 Pt 1):201-209.
doi pubmed - Hofmeyr GJ, Gulmezoglu AM, Pileggi C. Vaginal misoprostol for cervical ripening and induction of labour. Cochrane Database Syst Rev. 2010;2010(10):CD000941.
doi pubmed - Rankin K, Chodankar R, Raymond K, Bhaskar S. Misoprostol vaginal insert versus dinoprostone vaginal insert: A comparison of labour and delivery outcomes. Eur J Obstet Gynecol Reprod Biol. 2019;235:93-96.
doi pubmed - Rugarn O, Tipping D, Powers B, Wing DA. Induction of labour with retrievable prostaglandin vaginal inserts: outcomes following retrieval due to an intrapartum adverse event. BJOG. 2017;124(5):796-803.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Gynecology and Obstetrics is published by Elmer Press Inc.