| Journal of Clinical Gynecology and Obstetrics, ISSN 1927-1271 print, 1927-128X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Gynecol Obstet and Elmer Press Inc |
| Journal website https://jcgo.elmerpub.com |
Review
Volume 14, Number 1, January 2025, pages 1-13
Abnormal Uterine Bleeding: Saudi Guideline
Hisham Araba, j, Haifa Al-Turkib, Sameer Sendyc, Ayman Oraifd, Khalid Akkoure, Mohamad Qarif, Naemah Alshangeitig, Ghada Fouad Alyousifh, Namshah Alhajrii
aWomen & Fetal Health Program, Dr Arab Medical Center, Jeddah, Saudi Arabia
bOb/Gyn and Reproductive Medicine, Imam Abdulrahman Bin Faisal University, King Fahad Hospital, Haifa Medical Center, Khobar, Saudi Arabia
cObstetrics and Gynecology and Endoscopy, Alhabib Suwaidi Hospital, Riyadh, Saudi Arabia
dObstetrics and Gynecology and Reproductive Endocrinology, Minimal Invasive Gynecology, King AbdulAziz University, Jeddah, Saudi Arabia
eDepartment of Obstetrics and Gynecology, College of Medicine, King Saud University, Riyadh, Saudi Arabia
fDepartment of Hematology, King AbdulAziz University, Jeddah, Saudi Arabia
gObstetrics and Gynecology Services, Ministry of Health, Riyadh, Saudi Arabia
hFamily Medicine, Women’s Health, Imam Abdulrahman bin Faisal University, Dammam, Saudi Arabia
iObstetrics and Gynecology, Women Health, Riyadh, Saudi Arabia
jCorresponding Author: Hisham Arab, Women & Fetal Health Program, Dr Arab Medical Center, Jeddah 23433-8654, Saudi Arabia
Manuscript submitted November 3, 2024, accepted December 31, 2024, published online January 17, 2025
Short title: Saudi AUB Guideline
doi: https://doi.org/10.14740/jcgo1012
- Abstract
- Introduction
- Background
- Methods
- Surgical and Medical Treatment of AUB
- Discussion and Conclusion
- References
| Abstract | ▴Top |
The objective of the review was to provide Saudi clinicians with an evidence-based guideline that would aid them in the management of women with abnormal uterine bleeding (AUB). We put together a task force of Saudi experts to produce the guideline in 2024. We used the Grading of Recommendations, Assessment, Development and Evaluation (GRADE) approach to summarize the evidence and assess the quality. We presented our findings based on the International Federation of Gynecology and Obstetrics (FIGO) classification of AUB: the PALM-COEIN system. The goal of these recommendations is to stop acute bleeding, prevent heavy bleeding in the future, or improve the quality of life. This guideline summarized the recommendations based on pharmacological and surgical management of AUB. The task force’s recommendations are based on a thorough review of the literature and on expert opinion. There is a great need for research on the use of the different AUB treatment modules and cost analyses in the Saudi context.
Keywords: Abnormal uterine bleeding; Saudi Arabia; Guideline; Recommendations
| Introduction | ▴Top |
Abnormal uterine bleeding (AUB) is defined as any uterine bleeding with abnormalities affecting frequency, duration, or bleeding volume outside of pregnancy [1, 2]. AUB is a prevalent problem impacting a substantial portion of premenopausal women. According to the National Institute of Health and Care Excellence (NICE), heavy menses, a consequence of AUB, has a serious impact on women’s quality of life [2]. Women endure significant changes in their everyday activities, suffer financially due to reduced work productivity, and experience adverse health outcomes that lead to increased use of health care services [3].
The International Federation of Gynecology and Obstetrics (FIGO) approved the updated classification system for AUB, depicted by the acronym PALM-COEIN (Fig. 1). PALM refers to structural etiologies (P: polyp, A: adenomyosis, L: leiomyoma, M: malignancy and hyperplasia), while COEIN refers to non-structural etiologies (C: coagulopathy, O: ovulatory dysfunction, E: endometrial disorders, I: iatrogenic, N: not otherwise classified) [4, 5].
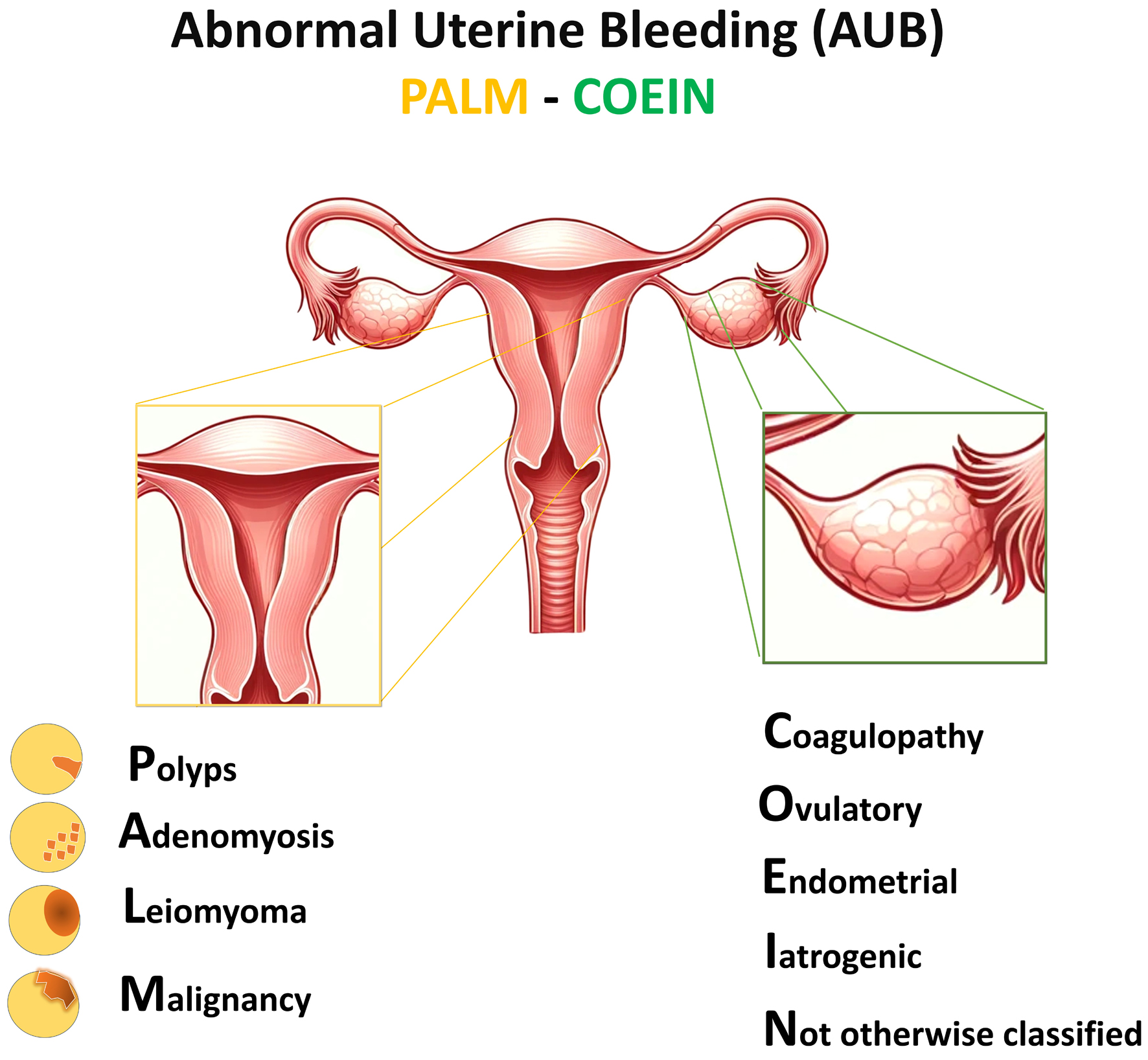 Click for large image | Figure 1. Abnormal uterine bleeding (AUB) PALM-COEIN classification. P: polyp, A: adenomyosis, L: leiomyoma, M: malignancy and hyperplasia, C: coagulopathy, O: ovulatory dysfunction, E: endometrial disorders, I: iatrogenic, N: not otherwise classified. |
The prevalence of AUB worldwide is estimated to be 10-30% among women of reproductive age [6]. In Saudi Arabia (SA), the number of studies reporting on prevalence of AUB is limited. A multicenter study assessing the prevalence of bleeding symptoms among young adults in 2021 reported menorrhagia in 28% of participants. When asked about heavy menstrual bleeding (HMB) of more than 7 days, 42% of those participants reported experiencing it [7]. A study in 2018 reported HMB by 24.5% of participants [8]. Another cross-sectional study identified 65% of their participants with HMB [9]. Despite the variation in numbers between the studies, we believe that the prevalence of AUB in SA is not far from the numbers reported internationally, if not more.
The current available interventions to treat AUB vary between pharmacological, interventional, or expectant management. A study by Spencer et al in 2017 estimated that in the United States (US), more than one billion US dollars is spent on a yearly basis to treat HMB [10]. Data on the cost of treating AUB in SA are lacking. One study from a center in Riyadh assessed the cost of treating iron deficiency anemia, a possible symptom of AUB, with iron saccharate and reported an annual total cost of 1.07 million Saudi Riyals [11], the cost from one center only in a country with a population of 30 million.
In 2018, the NICE in the United Kingdom issued a new national guideline for HMB in adults [2]. The American College of Obstetricians and Gynecologists (ACOG) in 2019 also released a guideline on this topic, with specific focus on adolescents [12]. To the best of our knowledge, no Saudi guideline for AUB has been developed so far.
The objective of this guideline is to deliberate treatment options based on the suspected causes, taking into consideration the age, cultural values, and preferences of Saudi patients. This guideline has been developed using the Grading of Recommendations, Assessment, Development and Evaluation (GRADE) methodology [13, 14] and relies on evidence from the literature. It has been crafted by a task force of Saudi experts using a multidisciplinary, collaborative approach to offer an updated and validated resource.
| Background | ▴Top |
Patient history and examination
The key to a successful investigation of women with chronic AUB is to obtain an accurate history that includes the establishment of the patient’s normal menstrual pattern, the features of AUB including timing, volume, and associated symptoms, and the impact that it has on her life (Table 1 [15, 16]). This can be achieved through a directed history and physical examination.
 Click to view | Table 1. Patient History and Examination for Suspected AUB |
Investigations
Laboratory testing
It is advisable to conduct laboratory assessments on the first visit for any patient experiencing AUB. All women with AUB should be screened for the presence of a systemic disorder of hemostasis. Additional tests are considered in patients suspected of von Willebrand disease (VWD) or other coagulopathies (Table 2 [17]).
 Click to view | Table 2. Laboratory Tests for Evaluating Patients With AUBa |
Imaging studies
These include transvaginal ultrasound (TVUS), magnetic resonance imaging (MRI), sonohysterography, and hysterosalpingography (HSG), which are detailed in Table 3.
 Click to view | Table 3. Imaging Modalities to Evaluate AUB |
Office studies
These office special investigations include endometrial biopsy, Pap smear, and office hysteroscopy outlined in Table 4.
 Click to view | Table 4. Office Special Investigations for AUB Evaluation |
The exact order of investigation may vary depending upon the clinical situation. Clinicians should also remember that more than one contributor to the onset of AUB may exist, and that it is common to identify structural lesions such as adenomyosis, some polyps, and leiomyomas (≥ type 3) that are asymptomatic. In these circumstances, clinical judgment and, in many instances, trials of therapy will be necessary to determine the clinically important findings.
| Methods | ▴Top |
A task force of five Saudi experts, mainly gynecologists, were charged with putting this guideline together. The guideline was then validated by four other experts including a gynecologist, a general practitioner, a hematologist, and a women-health specialist. The group also includes a patient representative and senior medical writer with statistical background. The committee initially determined the questions of interest, structured using PICO (P: patient, I: intervention, C: comparison, O: outcome) methodology. The outcomes of interest for our guideline included bleeding or menstrual blood loss, quality of life, any adverse events, and costs.
A search for the available systematic reviews and meta-analyses in the literature was performed in PubMed, Embase, MEDLINE and Cochrane databases on March 19, 2024. The search was limited to articles in English. We excluded studies that assessed herbal or alternative treatments for AUB.
We followed the GRADE approach for each PICO question, and we developed evidence profiles and tables [13]. The information was then shared with the task force and any additional information or input from the members was encouraged.
We assessed the quality of evidence using the GRADE approach [14]. When definitive scientific evidence was lacking, we recommended some practices on the basis of agreement between all the members (“expert opinion”).
The recommendations were graded and labelled as strong or weak. When the recommendations were strong, the task force formulated their recommendations using “the task force recommends” to indicate that it should be used for most patients. When the recommendation was weak, the task force formulated their recommendations using “the task force suggests” to maintain that the recommendation requires further decision-making and discussion.
Our target audience is clinicians, particularly obstetrics and gynecology (OBGYN) clinicians and family medicine practitioners who practice in SA. Policy makers can also benefit from these recommendations and can refer to them.
It is important to remember that when implementing this guideline, all physicians should utilize their own discretion, considering their individual expertise and the unique characteristics of their patient and their institution. This ensures the selection of the most appropriate treatment approach tailored to each particular patient.
| Surgical and Medical Treatment of AUB | ▴Top |
The recommendations detailed below by our task force assume that the physician treating the patient has confirmed their diagnosis (Table 1). Surgical treatment is considered in patients with uterine pathology, structural abnormalities such as endometrial polyps, or fibroids, or when medical treatment is contraindicated, failed or not tolerated by the patient. Therapeutic modalities that are unavailable in SA will not be mentioned in the recommendations.
Furthermore, it is important to highlight the importance of iron deficiency or iron deficiency anemia associated with AUB, particularly HMB, which should be treated with oral or intravenous iron as outlined by the Saudi Arabian Expert Consensus published by Arab et al in 2019 [18].
The scope of this guideline is to present the recommendations in nine different sections representing the etiological components of AUB as per FIGO classification.
AUB-polyp (AUB-P)
Approximately 10-20% of patients presenting with AUB will have an endometrial polyp [19, 20]. Polyps may be asymptomatic and incidentally identified either with imaging or histological or hysteroscopic assessment of the endometrial cavity. When symptomatic, they most commonly present with AUB [20] or postmenopausal bleeding.
Most polyps that are found incidentally in 5-15% of women are benign, and some may even regress on their own [21, 22]. Expectant management is therefore an option, depending on the patient’s desires and symptoms.
The most common route of managing AUB-P is through surgical interventions. Hysteroscopic resection of endometrial polyps, whether mechanically or electrosurgically, has been reported to be a relatively safe procedure with low rate of complications [23]. Polypectomy should particularly be conducted in women with postmenopausal bleeding as 6% of the women harbor atypical endometrial hyperplasia (EH) or cancer [24]. New technological advances in tissue removal systems (TRS) appear to be associated with quicker, more effective, less painful outcomes, and more readily obtainable tissue for histological examination [25]. In addition, outpatient treatment of AUB-P appears to be more cost-effective than inpatient treatment [24].
The use of blind polyp removal through cervical dilation and endometrial curettage (D&C) is outdated and risks incomplete excision, non-retrieval of specimens and uterine trauma.
Recommendations for AUB-P
The task force: 1) recommends the use of hysteroscopic uterine polypectomy for the management of patients with AUB-P (strong recommendation, moderate-quality evidence); 2) suggests expectant management if the patient desires and depending on the severity of her symptoms (conditional recommendation, moderate-quality evidence); 3) suggests a combination of surgical and medical treatment (for example, levonorgestrel-releasing intrauterine system (LNG-IUS), combined oral contraceptive (COC), etc. …) in women with AUB-P and persistent or heavy bleeding (conditional recommendation, moderate-quality evidence); 4) recommends office or outpatient hysteroscopic uterine polypectomy if feasible (strong recommendation, moderate-quality evidence); 5) suggests that non-electrical methods are preferred over the electrosurgical technique when available (conditional recommendation, moderate-quality evidence); and 6) recommends pathological testing of polyps after removal (strong recommendation, high-quality evidence).
AUB-adenomyosis (AUB-A)
Adenomyosis is characterized by the growth of endometrial cells into the myometrium, thus causing diffuse uterine extension, and one of its main symptoms is AUB [26, 27]. The coexistence of endometriosis or leiomyomas is well documented.
Medical management of AUB-A with non-steroidal anti-inflammatory drugs (NSAIDs) is frequently used to relieve symptoms. Two Cochrane reviews investigated the use of NSAIDs to treat dysmenorrhea and AUB and concluded that although NSAIDs are effective in reducing HMB, there is not enough evidence to conclude which NSAID would be more effective or safe to treat AUB-A [28, 29]. As for tranexamic acid (TA), another non-hormonal drug for the management of AUB, there is insufficient evidence on its effect in patients with AUB-A [30].
LNG-IUS devices are highly acceptable and cost-effective; however, it is not advisable to be used in the large uterus (> 9 cm) which is not an uncommon finding with adenomyosis [31, 32]. COCs are effective at reducing the pain and AUB-A, although LNG-IUS is much more efficient [32].
As second-line therapy for AUB-A, gonadotropin-releasing hormone agonist (GnRHa) and selective progesterone receptor modulators (SPRMs) such as mifepristone and ulipristal acetate (UPA) were found to be effective but with serious side effects [33].
The gold standard for the surgical treatment of AUB-A can be hysterectomy, despite the fact that adenomyosis affects a large proportion of women who are still in their reproductive age. Patients may not opt for hysterectomies as the surgery is invasive and is correlated with a number of potential complications. Medical management should be attempted before a hysterectomy is considered [34, 35].
A 2017 systematic review and meta-analysis investigating the findings of 30 observational trials, with more than 1,000 patients treated with uterine artery embolization (UAE) for adenomyosis, showed long-term and short-term improvement in HMB and dysmenorrhea [36]. The use of UAE should be applied while taking into consideration the patients’ symptoms and providing the patient with extensive counselling.
A novel non-invasive treatment of adenomyosis is high-intensity focused ultrasound (HIFU) ablation. A study on combination therapy of HIFU, mifepristone, and LNG-IUS concluded that it is an effective, safe, and inexpensive treatment for patients with symptomatic adenomyosis who refuse hysterectomies, but has a 20% relapse rate [33].
Given its high acceptability rate among women, endometrial ablation (EA) could be a well-received therapeutic option amongst perimenopausal women suffering from AUB-A without pelvic pain [37, 38].
Adenomyomectomy is a complex procedure that requires an experienced surgeon. While focal adenomyosis is responsive to minimally invasive surgery, the diffuse type requires open surgery [34].
Recommendations for AUB-A
The task force: 1) recommends the use of LNG-IUS as effective first-line therapy in women who are not planning on getting pregnant and suffering from AUB-A (strong recommendation, moderate-quality evidence); 2) recommends the use of GnRHa as second-line treatment with add-back therapy in patients with AUB-A when oral progestins are not efficacious or not tolerated by the patients, or when patients desire to remain fertile (strong recommendation, moderate-quality evidence); 3) suggests the use of COCs or oral progestins as an alternative to LNG-IUS (conditional recommendation, low-quality evidence); 4) suggests that NSAIDs could be considered for managing recurrent exacerbations of AUB-A in women already receiving optimized hormonal treatment or in women seeking pregnancy who are not undergoing any treatment other than symptomatic relief (conditional recommendation, moderate-quality evidence); 5) recommends the use of UAE to treat AUB-A in women who have failed medical treatment or where medical treatment is contraindicated after proper counselling with focus on future fertility (strong recommendation, moderate-quality evidence); 6) suggests the use of HIFU for AUB-A in women who have completed childbearing (conditional recommendation, low-quality evidence); 7) suggests a surgical approach to focal or diffuse adenomyomectomy (laparoscopic, robotic, or open) (conditional recommendation, low-quality evidence); and 8) recommends hysterectomy for AUB-A which can be offered to women if they failed or are not good candidates for medical treatment or opted for definitive surgical management and after appropriate counselling regarding fertility, risks, benefits, and alternative treatments (strong recommendation, medium-quality evidence).
AUB-leiomyoma (AUB-L)
Leiomyomas are common and nearly 20-50% of patients with these fibroids experience symptoms, such as AUB, infertility, pelvic pain, and miscarriages [39]. Most fibroids degenerate on their own, therefore expectant management could be an option in premenopausal women depending on the severity of symptoms [40].
There is limited evidence on the effect of oral contraceptives on AUB-L; however, they have been shown to reduce menstrual bleeding in the short-term and may inhibit the development of leiomyomas [41]. The data available however are not enough to support the use of oral progestogens or LNG-IUS in the treatment of women with AUB-L [42].
A systematic review and meta-analysis by Telek et al revealed that oral GnRH antagonists seem to be effective for AUB-M and for improving quality of life. The safety profile is acceptable for short-term use, but lipid metabolism is affected [43]. Another systematic review by Rovelli et al revealed statistically significant improvement in AUB-L in 100% of the relugolix studies, 80% of the elagolix studies, and 0% in the linzagolix studies [44].
The effects of danazol, and SPRMs such as mifepristone and UPA, have been described in the literature; however, these medications are not available in the Saudi market, and hence will not be discussed here.
Hysterectomy is the most effective treatment for symptomatic leiomyomas, especially in women who have completed their families. Hysterectomy might also be indicated in menopausal women with enlarging asymptomatic fibroids.
An alternative to a hysterectomy is a myomectomy, which will retain a woman’s uterus. It is estimated that there is a 15% chance of recurrence in women undergoing this procedure, and that 10% of these women will ultimately need a hysterectomy within 5 - 10 years [45]. A meta-analysis found that rates of major complications, pregnancy rates and outcomes, and recurrence of myoma in laparoscopic and laparotomic myomectomy were comparable [46]. Uterine fibroids FIGO type 0, 1 and 2 can be removed hysteroscopically in an office setting or operative theaters using different techniques such as mini-resectoscope, TRS, or diode laser. Taking into consideration the low cost, minimal risk of complications and discomfort correlated with hysteroscopic myomectomy, the resection of such lesions should always be considered.
The use of blind D&C is not recommended [25]. When access to a center with hysteroscopy is not available, patients should be referred to other centers where this procedure is accessible.
Recommendations for AUB-L
The task force: 1) recommends individualized treatment for women with AUB-L, taking into considerations the symptoms, size and location of the leiomyoma, the desire to preserve fertility, age, treatment available, physician’s preference, and cost (strong recommendation, high-quality evidence); 2) suggests expectant management of AUB-L in premenopausal women depending on the severity of their symptoms and risk of malignancy (conditional recommendation, low-quality evidence); 3) recommends myomectomy (laparoscopic, robotic, open) in women with AUB-L when indicated (strong recommendation, high-quality evidence); 4) recommends the use of in-bag morcellation when doing a minimally invasive myomectomy (strong recommendation, high-quality evidence); 5) recommends hysteroscopic myomectomy as a first-line surgical treatment in women with AUB-L with symptomatic intracavitary fibroids FIGO 0-1-2 (strong recommendation, moderate-quality evidence); 6) suggests medical management for women with AUB-L (conditional recommendation, moderate-quality evidence); 7) recommends hysterectomy in women with AUB-L who are symptomatic, after appropriate counselling regarding fertility, risks, benefits, and alternative treatments (strong recommendation, high-quality evidence); and 8) recommends hysterectomy for menopausal women who have rapidly enlarging fibroids or imaging suspicious for malignancy (strong recommendation, high-quality evidence).
AUB-malignancy (AUB-M)
Finding a pelvic tumor in women who are symptomatic or asymptomatic raises the concern of malignancy. AUB can be both a symptom or a precursor of endometrial malignancy [47]. A study by Grubman et al found that physicians who do not adhere to evidence-based evaluation and management of premenopausal AUB could contribute to avoidable cases and delayed diagnosis of endometrial malignancy [48].
The excessive production of cells in the endometrium, otherwise known as EH, usually precedes the development of endometrial cancer [49]. A systematic review by Mittermeier et al found that the use of an LNG-IUS device as treatment of EH with or without atypia for the duration of 6 months is possibly more effective than non-intrauterine progestogens (odds ratio (OR) 2.94; P < 0.001) or no treatment (OR 78.41; P < 0.001) [50].
Once AUB-M is diagnosed, the patient should be referred to a gynecologist oncologist for further management.
Recommendations for AUB-M
The task force: 1) recommends the use of a minimally invasive surgical approach in patients with histopathological proven endometrial carcinoma (strong recommendation, high-quality evidence); 2) recommends referral to a gynecologist oncologist and following the proper protocol for management of malignancy (strong recommendation, high-quality evidence); 3) recommends hysterectomy as a standard of care for EH with atypia in post-menopausal women and after appropriate counselling regarding fertility, risks, benefits, and alternative treatments (strong recommendation, moderate-quality evidence); 4) recommends medical treatment in women desiring fertility with grade 1 endometroid adenocarcinoma of the endometrium provided that they fulfill the criteria (no myometrial invasion, no suspicious lymph node metastasis), a gynecologist oncologist should be consulted (strong recommendation, high-quality evidence); 5) recommends the use of LNG-IUS device as first-line treatment to regress EH without atypia (strong recommendation, high-quality evidence); and 6) suggests the use of oral progestins to regress EH without atypia if LNG-IUS cannot be used or contraindicated (conditional recommendation, moderate-quality evidence).
AUB-coagulopathy (AUB-C)
The term AUB-C has been used to describe any hemostasis disorders of a systemic nature and that presents as AUB or contributes to the manifestation of AUB along with other existent conditions [51]. Women who require anticoagulation as a lifelong treatment are placed in this category according to the new FIGO classification system.
The management of women with AUB-C usually involves the use of a pharmacological approach. TA may be given to women with AUB-C even before a diagnosis is made. Desmopressin can be started with or without coagulation factor VIII (FVIII) in consultation with a hematologist [52].
A systematic review by Ray and Ray in 2016 reported that the findings from two studies agree that there might be a reduction in mean blood loss (MBL) with the use of desmopressin as compared to placebo, despite the fact that the findings were not significant [53].
Studies have reported a 10-62% incidence of AUB-C in adolescents [54]. Adolescents and women who wish to retain their fertility but not planning to get pregnant in the near future should also be placed on conservative management. This would involve the use of COCs as first-line therapy [55]. Other treatment options include LNG-IUS, which has been proven to be well tolerated and effective in controlling AUB [56, 57].
Women who do not wish to retain their fertility or who have completed childbearing could resort to surgical treatment for AUB-C. Procedures such as EA or hysterectomy can be opted for and are an option to be considered particularly when uterine fibroid tumors have been diagnosed [52].
NSAIDs should not be used as a therapy for AUB-C in general, because they affect platelet function and may further increase menstrual loss in those women with undiagnosed bleeding disorders. Additionally, NSAIDs should be shunned completely in women with diagnosed VWD and menorrhagia [52].
Recommendations for AUB-C
The task force: 1) recommends consulting with a hematologist in women with AUB-C to tailor treatment to the individual patient and the clinical situation (strong recommendation, high-quality evidence); 2) recommends the use of TA in women with AUB-C who wish to preserve their fertility and get pregnant soon (strong recommendation, high-quality evidence); 3) recommends the use of COC or LNG-IUS as first-line therapy in women with AUB-C who wish to preserve their fertility but not planning on getting pregnant soon (strong recommendation, high-quality evidence); 4) recommends not using NSAIDs as treatment in women with AUB-C (strong recommendation, high-quality evidence); 5) suggests minimally invasive surgical management when all medical management has failed and after appropriate counselling regarding fertility, risks, benefits, and alternative treatments (conditional recommendation, moderate-quality evidence); and 6) recommends hormonal therapy, preferably COC for adolescents with AUB-C (strong recommendation, moderate-quality evidence).
AUB-ovulatory dysfunction (AUB-O)
The underlying causes of AUB-O vary amongst women. They can be categorized into four types: hypothalamic, pituitary, ovarian and PCOS. AUB-O may occur at differing episodes and may be transient, a situation that is commonly observed in adolescent women. In such cases, expectant management should be utilized as long as the symptoms have no great impact on quality of life [58].
Treatment options for AUB-O are medical rather than surgical. The choice of treatment depends on the goals of the therapy set for each patient. COCs or progestin alone, which would include LNG-IUS, progestogen-only pill, or cyclical oral progestogens such as norethisterone, and dydrogesterone are effective in treating AUB-O [17]. Two systematic reviews investigated the use of COCs or progestogens for the treatment of AUB-O; the first did not find any randomized trials evaluating the use of oral progestins or combined hormonal contraceptives specifically for treating AUB-O [59]; while the second reported that LNG-IUS is effective in treating AUB and should be an option for treatment across all age groups [60].
Cyclical oral progestogens on the other hand have shown promising results in the treatment of AUB-O. A systematic review conducted in 2019 in women with HMB only assessed norethisterone and medroxyprogesterone acetate, with no mention of dydrogesterone [61]. The review reported low-quality evidence in terms of use of norethisterone for short-cycle or long-cycle therapy and could not make inferences about the potential use for the treatment of HMB [61]. Two studies comparing norethisterone and dydrogesterone treatment in AUB revealed that both treatments can be used efficiently for AUB-O [62, 63]. However, dydrogesterone is a potent progestogen and has a high selectivity for progesterone receptors with no or negligible agonistic activity at androgen, glucocorticoid, and mineralocorticoid receptors. At the same time, norethisterone is partially androgenic, and a significant amount of it gets converted to estrogen (ethinyl estradiol) [64]. Hence, dydrogesterone is a better option when these two effects are to be avoided like in adolescents or when estrogen is contraindicated. A literature review for clinical trials on dydrogesterone and AUB-O revealed mostly observational trials ensuring remarkable regularization of menstrual cycles in dydrogesterone-treated women with AUB-O [65-68]. A study by Wang et al in 2020 evaluated the effectiveness of dydrogesterone in AUB-O and reported its effectiveness in achieving a regular menstrual cycle after three treatment cycles of dydrogesterone in 80.9% of women [69].
Lifestyle changes such as exercising and losing weight have also been shown to improve anovulation in women with AUB-O [70, 71]. It has been speculated that weight loss would lead to the return of regular ovulation by normalizing testosterone levels [71].
Resorting to EA is not recommended as first-line therapy for AUB-O. Women who chose EA as treatment need to be extensively counselled about its side effects and the risks relevant to detecting endometrial cancer prospectively.
A hysterectomy may be considered when an evaluation of the endometrium cannot be clearly conducted after EA to rule-out the possibility of endometrial cancer. In addition, women with AUB-O who have completed childbearing and who have not responded or had complications with medical treatment, can be candidates for hysterectomy without cervical preservation [17].
During adolescence, anovulation is the most common reason for AUB.
Adolescents with chronic anovulation generally respond well to outpatient medical therapy with exogenous steroids, such as COCs or oral progestins.
Recommendations for AUB-O
The task force: 1) recommends lifestyle modifications in overweight and obese women with AUB-O (strong recommendation, moderate-quality evidence); 2) recommends the use of oral progestin, namely norethisterone and dydrogesterone, and combined hormonal contraception to manage women with AUB-O (strong recommendation, moderate-quality evidence); 3) recommends the use of LNG-IUS to treat AUB-O across all age groups after appropriate counselling regarding fertility (strong recommendation, moderate-quality evidence); 4) suggests surgical treatment only when medical therapy fails, contraindicated, or is not tolerated by the patient (conditional recommendation, moderate-quality evidence); 5) recommends not using EA as first-line treatment in women with AUB-O (strong recommendation, moderate-quality evidence); 6) suggests hysterectomy in women with AUB-O who have completed childbearing and when medical treatment has failed (conditional recommendation, moderate-quality evidence); and 7) recommends the use of oral progestin therapy or low-dose combination hormonal contraceptives in adolescents with AUB-O (strong recommendation, moderate-quality evidence).
AUB-endometrial dysfunction (AUB-E)
Any bleeding that happens in women who have regular menstrual cycles, who have structural abnormalities in the uterus, or any evidence of coagulopathy is due to an endometrial disorder.
First-line medical treatment for AUB-E involves the use of LNG-IUS device, especially in women who do not plan on getting pregnant presently. When compared to EA, LNG-IUS has been reported to have comparable rates of reducing menstrual blood loss and improving quality of life [72, 73].
TA appears to be the safest and most effective non-hormonal treatment for AUB-E. Its cyclical administration during menstruation makes it convenient for women who are trying to conceive. Concomitant use of NSAIDs and TA might be of advantage in associated dysmenorrhea [58].
The use of surgical techniques to manage AUB-E is only advisable when all medical management has failed. EA could be utilized in women who have finalized childbearing. Studies have shown that EA could lead to an 80-90% reduction in blood loss after 1 year [74].
Recommendations for AUB-E
The task force: 1) recommends the use of LNG-IUS in women with AUB-E who do not wish to conceive in the near future (strong recommendation, high-quality evidence); 2) recommends the use of TA concomitantly with NSAIDs in women with AUB-E who wish to conceive in the near future (strong recommendation, moderate-quality evidence); 3) recommends the use of combined estrogen and oral progestin contraception formulations in women with AUB-E when LNG-IUS is not an option (strong recommendation, high-quality evidence); 4) recommends reverting to surgical treatment only when all medical treatment has failed (strong recommendation, high-quality evidence); 5) recommends EA in women with AUB-E who have finalized childbearing and after appropriate counselling regarding fertility, risks, benefits, and alternative treatments (strong recommendation, high-quality evidence); 6) suggests a hysterectomy in women with AUB-E who failed other treatment options and after appropriate counselling regarding fertility, risks, benefits, and alternative treatments (conditional recommendation, moderate-quality evidence); and 7) suggests expectant management in postmenopausal women with a negative endometrial biopsy (conditional recommendation, moderate-quality evidence).
AUB-iatrogenic (AUB-I)
AUB-I usually occurs as a result of exogenous treatments such as medications or medical devices that affect the endometrium directly. These treatments include estrogen or progestin therapy via systemic intake or intrauterine routes, GnRHa, selective estrogen receptor modulators (SERMs), and rarely SPRMs.
AUB-I could resolve on its own especially when certain therapeutic options are initiated. The use of GnRH modulators, for example, could cause bleeding or spotting in women once they commence therapy. The symptoms usually subside however, and patients should be counseled regarding this possibility [75].
Recommendations for AUB-I
The task force: 1) recommends reviewing all medications and selecting medication with least side effects in terms of bleeding without affecting the main indication for that treatment, after proper consultation with prescribing physician (strong recommendation, high-quality evidence); 2) recommends counseling patients about the potential of bleeding, especially when certain therapeutic options are initiated (strong recommendation, high-quality evidence); and 3) suggests considering surgical management if all attempts to manage AUB-I had failed (conditional recommendation, moderate-quality evidence).
AUB-not otherwise classified (AUB-N)
Women who experience AUB-N fall under the category where the underlying pathology or condition does not fit the FIGO classification. Examples of conditions include arteriovenous (A-V) malformations, myometrial hypertrophy, chronic endometritis, and isthmoceles [4, 5].
The treatment options for AUB-N depend on the cause of the bleeding and decision-to-treat should take into consideration the woman’s preference and their desire for future childbearing. The preferred treatment is primarily medical and resorting to surgical treatment should only be considered when all medical treatment has failed or when the underlying cause requires a surgical intervention or when the woman with AUB-N desires surgical therapy.
The first-line recommended treatment for AUB-N is LNG-IUS in women who do not desire to conceive in the coming future. If this device is contraindicated, or if the woman with AUB-N wishes to remain fertile, then COCs are recommended [58].
Cyclic or predictable AUB-N can be well managed with TA and NSAIDs. Some conditions require surgery, such as A-V malformations, where surgical management using UAE or even a hysteroscopy may be indicated. As for isthmoceles, then hysteroscopic reshaping or excision and repair via a vaginal or abdominal approach, either laparoscopic or open might be the preferred approach [58].
Recommendations for AUB-N
The task force: 1) recommends treatment of women with AUB-N based on the cause and patients’ preference (strong recommendation, high-quality evidence); 2) recommends the use of LNG-IUS or COC depending on patient presentation and preference and after proper counselling (strong recommendation, high-quality evidence); 3) recommends the use of TA and NSAIDs in women with AUB-N with predictable bleeding timing and patterns (strong recommendation, high-quality evidence); 4) recommends management using UAE in women with A-V malformations (strong recommendation, high-quality evidence); 5) recommends hysteroscopic reconstruction or excision via minimally invasive or open routes in women with isthmoceles (strong recommendation, moderate-quality evidence); and 6) suggests a hysterectomy only when all medical interventions have failed or are not available and after appropriate counselling regarding fertility, risks, benefits, and alternative treatments (conditional recommendation, high-quality evidence).
| Discussion and Conclusion | ▴Top |
AUB is a very common condition amongst women of reproductive age. The major downside of this condition is that it affects the daily livelihood and quality of life of women suffering from it and interferes with their day-to-day activities. Treatment options for AUB depend on the underlying cause of the bleeding and could either involve medical or surgical intervention.
Our goal is to develop a guideline that would provide clinicians with the proper tools for decision making and standardize treatment of AUB in SA. The task force took into consideration the local context and experience of its members when drafting the recommendations in an attempt to make sure they are applicable and acceptable likewise.
Clinicians, healthcare organizations, patients, and other stakeholders should be aware of and understand our recommendations, so they can put them into practice. The recommendations that we have listed should not be applied without taking into consideration the unique features and circumstances surrounding each patient. Therefore, it is important to emphasize that these recommendations should not be applied in a blanket fashion by clinicians, patients, healthcare organizations, third-party payers, institutional review committees, courts, or other stakeholders. It is also important to consider the patients’ values and preferences as part of the decision-making process and to thoroughly counsel the patient, particularly about fertility and desire for conception and any side effects that the intervention could cause.
The task force took note of much-needed research especially in the Saudi context while drafting these recommendations. The data available on cost-effectiveness and patient preferences are lacking in SA. The task force recommends that additional research about the acceptability and application of medical treatment for AUB be conducted, especially invasive surgical interventions and their assimilation among Saudi women. Moreover, further investigation into the unmet needs of women with AUB should be considered and their outlook regarding living with this condition should be explored.
Overall, this evidence-based guideline was set forth by a group of experts in the field, and experts with specialties of relevance to AUB such as hematology and oncology were involved to enhance the quality and widen the scope of the recommendations. The recommendations were drafted with the highest medical standards in mind and supported by the Saudi Ministry of Health.
Acknowledgments
The task force would like to acknowledge Ms. Rola El Rassi for contributing to documenting and compiling the guideline.
Financial Disclosure
The task force attests that this guideline is an independent effort that has not been influenced by any external party. The scientific work was backed by the support of Hologic, INC.
Conflict of Interest
The authors declare that they have no conflict of interest relevant to the content of this manuscript. The authors have no relevant financial or non-financial interests to disclose.
Informed Consent
Not applicable.
Author Contributions
Hisham Arab contributed to the project development, methodology, supervision, manuscript writing; manuscript review and editing; Haifa Al-Turki contributed to the project development, manuscript writing; Sameer Sendy contributed to the project development, manuscript writing; Ayman Oraif contributed to the project development, manuscript writing; Khalid Akkour contributed to the project development, manuscript writing; Mohamad Qari contributed to the validation, manuscript review and editing; Naemah Alshangeiti contributed to the validation, manuscript review and editing; Ghada Alyousif contributed to the validation, manuscript review and editing; Namshah Alhajri contributed to the validation, manuscript review and editing.
Data Availability
The data supporting the findings of this study are available from the corresponding author upon reasonable request.
Abbreviations
ACOG: American College of Obstetricians and Gynecologists; AUB: abnormal uterine bleeding; AUB-A: AUB-adenomyosis; AUB-C: AUB-coagulopathy; AUB-E: AUB-endometrial dysfunction; AUB-I: AUB-iatrogenic; AUB-L: AUB-leiomyoma; AUB-M: AUB-malignancy; AUB-N: AUB-not otherwise classified; AUB-P: AUB-polyp; A-V: arteriovenous; COC: combined oral contraceptive; D&C: dilatation and curettage; DHEA-S: dehydroepiandrosterone sulfate; EA: endometrial ablation; EH: endometrial hyperplasia; FIGO: International Federation of Gynecology and Obstetrics; FSH: follicle-stimulating hormone; FVIII: coagulation factor VIII; GnRHa: gonadotropin-releasing hormone agonist; GRADE: Grading of Recommendations, Assessment, Development and Evaluation; HIFU: high-intensity focused ultrasound; HMB: heavy menstrual bleeding; HSG: hysterosalpingography; LH: luteinizing hormone; LNG-IUS: levonorgestrel-releasing intrauterine system; MBL: mean blood loss; MRI: magnetic resonance imaging; NICE: National Institute of Health and Care Excellence; NSAIDs: non-steroidal anti-inflammatory drugs; OBGYN: obstetrics and gynecology; OR: odds ratio; PALM-COEIN: P, polyp, A, adenomyosis, L, leiomyoma, M, malignancy and hyperplasia, C, coagulopathy, O, ovulatory dysfunction, E, endometrial disorders, I, iatrogenic, N, not otherwise classified; PCOS: polycystic ovary syndrome; PICO: P, patient, I, intervention, C, comparison, O, outcome; SERM: selective estrogen receptor modulator; SIS: saline infusion sonography; SPRM: selective progesterone receptor modulator; SSRIs: selective serotonin reuptake inhibitors; STI: sexually transmitted infection; TA: tranexamic acid; 3D: three-dimensional; TRS: tissue removal systems; TVS: transvaginal sonography; TVUS: transvaginal ultrasound; 2D: two-dimensional; UAE: uterine artery embolization; UPA: ulipristal acetate; VWD: von Willebrand disease
| References | ▴Top |
- Fraser IS, Critchley HO, Broder M, Munro MG. The FIGO recommendations on terminologies and definitions for normal and abnormal uterine bleeding. Semin Reprod Med. 2011;29(5):383-390.
doi pubmed - NICE. Heavy menstrual bleeding: assessment and management. 2018.
- Wouk N, Helton M. Abnormal uterine bleeding in premenopausal women. Am Fam Physician. 2019;99(7):435-443.
pubmed - Munro MG, Critchley HO, Broder MS, Fraser IS, Disorders FWGoM. FIGO classification system (PALM-COEIN) for causes of abnormal uterine bleeding in nongravid women of reproductive age. Int J Gynaecol Obstet. 2011;113(1):3-13.
doi pubmed - Munro MG, Critchley HOD, Fraser IS, Committee FMD. The two FIGO systems for normal and abnormal uterine bleeding symptoms and classification of causes of abnormal uterine bleeding in the reproductive years: 2018 revisions. Int J Gynaecol Obstet. 2018;143(3):393-408.
doi pubmed - Liu Z, Doan QV, Blumenthal P, Dubois RW. A systematic review evaluating health-related quality of life, work impairment, and health-care costs and utilization in abnormal uterine bleeding. Value Health. 2007;10(3):183-194.
doi pubmed - AlSaleh KA, Al-Numair NS, Alsuaiman A, Zolaly M, Khojah OT, AlZahrani FM, Siddiqui K, et al. Prevalence of bleeding symptoms among young adults in Saudi Arabia, a national survey. Medicine (Baltimore). 2021;100(43):e27513.
doi pubmed - Owaidah T, Saleh M, Alzahrani H, Abu-Riash M, Al Zahrani A, Almadani M, Alsulaiman A, et al. Prevalence of bleeding symptoms among adolescents and young adults in the capital city of Saudi Arabia. Adv Hematol. 2018;2018:1858241.
doi pubmed - Alsalman M, Albarak A, Busaleh F, Alshaikh S, Alluwaim M, Busaleh M, Albarrak A. Heavy menstrual bleeding awareness among Saudi female population and clinical implications. Health Sci Rep. 2021;4(1):e244.
doi pubmed - Spencer JC, Louie M, Moulder JK, Ellis V, Schiff LD, Toubia T, Siedhoff MT, et al. Cost-effectiveness of treatments for heavy menstrual bleeding. Am J Obstet Gynecol. 2017;217(5):574.e1-e9.
doi pubmed - Alhejazi A, et al. PIH24 cost of treating iron deficiency Anaemia (IDA) with ferric carboxymaltose versus iron saccharate in heavy uterine bleeding (HUB) patients in the kingdom of Saudi Arabia. Value in Health. 2019;22:S186.
- ACOG Committee Opinion No. 785, screening and management of bleeding disorders in adolescents with heavy menstrual bleeding: correction. Obstet Gynecol. 2023;141(1):228.
doi pubmed - Guyatt G, Oxman AD, Akl EA, Kunz R, Vist G, Brozek J, Norris S, et al. GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. J Clin Epidemiol. 2011;64(4):383-394.
doi pubmed - Neumann I, Santesso N, Akl EA, Rind DM, Vandvik PO, Alonso-Coello P, Agoritsas T, et al. A guide for health professionals to interpret and use recommendations in guidelines developed with the GRADE approach. J Clin Epidemiol. 2016;72:45-55.
doi pubmed - Davis E, Sparzak PB. Abnormal uterine bleeding. In: StatPearls. Treasure Island (FL). 2024.
pubmed - Whitaker L, Critchley HO. Abnormal uterine bleeding. Best Pract Res Clin Obstet Gynaecol. 2016;34:54-65.
doi pubmed - ACOG committee opinion no. 557: Management of acute abnormal uterine bleeding in nonpregnant reproductive-aged women. Obstet Gynecol. 2013;121(4):891-896.
doi pubmed - Arab HA, Almomen A, Kashgari FA, Elawad MM, et al. Practical guidance on managing iron deficiency in women of childbearing age - a Saudi Arabian Expert Consensus. Med J Obstet Gynecol. 2019;7(1).
- Bougie O, Randle E, Thurston J, Magee B, Warshafsky C, Rittenberg D. Guideline No. 447: diagnosis and management of endometrial polyps. J Obstet Gynaecol Can. 2024;46(3):102402.
doi pubmed - Dreisler E, Stampe Sorensen S, Ibsen PH, Lose G. Prevalence of endometrial polyps and abnormal uterine bleeding in a Danish population aged 20-74 years. Ultrasound Obstet Gynecol. 2009;33(1):102-108.
doi pubmed - DeWaay DJ, Syrop CH, Nygaard IE, Davis WA, Van Voorhis BJ. Natural history of uterine polyps and leiomyomata. Obstet Gynecol. 2002;100(1):3-7.
doi pubmed - Lee SC, Kaunitz AM, Sanchez-Ramos L, Rhatigan RM. The oncogenic potential of endometrial polyps: a systematic review and meta-analysis. Obstet Gynecol. 2010;116(5):1197-1205.
doi pubmed - Lieng M, Istre O, Qvigstad E. Treatment of endometrial polyps: a systematic review. Acta Obstet Gynecol Scand. 2010;89(8):992-1002.
doi pubmed - Cooper NA, Clark TJ, Middleton L, Diwakar L, Smith P, Denny E, Roberts T, et al. Outpatient versus inpatient uterine polyp treatment for abnormal uterine bleeding: randomised controlled non-inferiority study. BMJ. 2015;350:h1398.
doi pubmed - Clark TJ, Stevenson H. Endometrial Polyps and Abnormal Uterine Bleeding (AUB-P): What is the relationship, how are they diagnosed and how are they treated? Best Pract Res Clin Obstet Gynaecol. 2017;40:89-104.
doi pubmed - Etrusco A, Barra F, Chiantera V, Ferrero S, Bogliolo S, Evangelisti G, Oral E, et al. Current medical therapy for adenomyosis: from bench to bedside. Drugs. 2023;83(17):1595-1611.
doi pubmed - Benetti-Pinto CL, Mira TAA, Yela DA, Teatin-Juliato CR, Brito LGO. Pharmacological treatment for symptomatic adenomyosis: a systematic review. Rev Bras Ginecol Obstet. 2019;41(9):564-574.
doi pubmed - Bofill Rodriguez M, Lethaby A, Farquhar C. Non-steroidal anti-inflammatory drugs for heavy menstrual bleeding. Cochrane Database Syst Rev. 2019;9(9):CD000400.
doi pubmed - Marjoribanks J, Ayeleke RO, Farquhar C, Proctor M. Nonsteroidal anti-inflammatory drugs for dysmenorrhoea. Cochrane Database Syst Rev. 2015;2015(7):CD001751.
doi pubmed - Dason ES, Maxim M, Sanders A, Papillon-Smith J, Ng D, Chan C, Sobel M. Guideline No. 437: diagnosis and management of adenomyosis. J Obstet Gynaecol Can. 2023;45(6):417-429.e411.
doi pubmed - Mansukhani N, Unni J, Dua M, Darbari R, Malik S, Verma S, Bathla S. Are women satisfied when using levonorgestrel-releasing intrauterine system for treatment of abnormal uterine bleeding? J Midlife Health. 2013;4(1):31-35.
doi pubmed - Shaaban OM, Ali MK, Sabra AM, Abd El Aal DE. Levonorgestrel-releasing intrauterine system versus a low-dose combined oral contraceptive for treatment of adenomyotic uteri: a randomized clinical trial. Contraception. 2015;92(4):301-307.
doi pubmed - Zhu H, Ma Q, Dong G, Yang L, Li Y, Song S, Mu Y. Clinical evaluation of high-intensity focused ultrasound ablation combined with mifepristone and levonorgestrel-releasing intrauterine system to treat symptomatic adenomyosis. Int J Hyperthermia. 2023;40(1):2161641.
doi pubmed - Osada H. Uterine adenomyosis and adenomyoma: the surgical approach. Fertil Steril. 2018;109(3):406-417.
doi pubmed - Thurston J, Murji A, Scattolon S, Wolfman W, Kives S, Sanders A, Leyland N. No. 377-Hysterectomy for Benign Gynaecologic Indications. J Obstet Gynaecol Can. 2019;41(4):543-557.
doi pubmed - de Bruijn AM, Smink M, Lohle PNM, Huirne JAF, Twisk JWR, Wong C, Schoonmade L, et al. Uterine Artery Embolization for the Treatment of Adenomyosis: A Systematic Review and Meta-Analysis. J Vasc Interv Radiol. 2017;28(12):1629-1642.e1.
doi pubmed - Lou J, Huang X, Zhang L, Xu P, Zhang X, Chen Z. [The second generation endometrial ablation (NovaSure) improves efficacy of levonorgestrel-releasing intrauterine system in management of adenomyosis]. Zhejiang Da Xue Xue Bao Yi Xue Ban. 2019;48(2):136-141.
doi pubmed - Philip CA, Le Mitouard M, Maillet L, de Saint-Hilaire P, Huissoud C, Cortet M, Dubernard G. Evaluation of NovaSure (R) global endometrial ablation in symptomatic adenomyosis: A longitudinal study with a 36 month follow-up. Eur J Obstet Gynecol Reprod Biol. 2018;227:46-51.
doi pubmed - Buttram VC, Jr., Reiter RC. Uterine leiomyomata: etiology, symptomatology, and management. Fertil Steril. 1981;36(4):433-445.
doi pubmed - Carranza-Mamane B, Havelock J, Hemmings R, Reproductive E, Infertility C, Special C. The management of uterine fibroids in women with otherwise unexplained infertility. J Obstet Gynaecol Can. 2015;37(3):277-285.
doi pubmed - Moroni RM, Martins WP, Dias SV, Vieira CS, Ferriani RA, Nastri CO, Brito LG. Combined oral contraceptive for treatment of women with uterine fibroids and abnormal uterine bleeding: a systematic review. Gynecol Obstet Invest. 2015;79(3):145-152.
doi pubmed - Sangkomkamhang US, Lumbiganon P, Laopaiboon M, Mol BW. Progestogens or progestogen-releasing intrauterine systems for uterine fibroids. Cochrane Database Syst Rev. 2013;(2):CD008994.
doi pubmed - Telek SB, Gurbuz Z, Kalafat E, Ata B. Oral gonadotropin-releasing hormone antagonists in the treatment of uterine myomas: a systematic review and network meta-analysis of efficacy parameters and adverse effects. J Minim Invasive Gynecol. 2022;29(5):613-625.
doi pubmed - Rovelli RJ, Cieri-Hutcherson NE, Hutcherson TC. Systematic review of oral pharmacotherapeutic options for the management of uterine fibroids. J Am Pharm Assoc (2003). 2022;62(3):674-682.e675.
doi pubmed - Yoo EH, Lee PI, Huh CY, Kim DH, Lee BS, Lee JK, Kim D. Predictors of leiomyoma recurrence after laparoscopic myomectomy. J Minim Invasive Gynecol. 2007;14(6):690-697.
doi pubmed - Jin C, Hu Y, Chen XC, Zheng FY, Lin F, Zhou K, Chen FD, et al. Laparoscopic versus open myomectomy—a meta-analysis of randomized controlled trials. Eur J Obstet Gynecol Reprod Biol. 2009;145(1):14-21.
doi pubmed - Clarke MA, Long BJ, Sherman ME, Lemens MA, Podratz KC, Hopkins MR, Ahlberg LJ, et al. Risk assessment of endometrial cancer and endometrial intraepithelial neoplasia in women with abnormal bleeding and implications for clinical management algorithms. Am J Obstet Gynecol. 2020;223(4):549.e1-e13.
doi pubmed - Grubman J, Mora V, Nguyen M, Ladwig N, Chen LM, Jacoby V. Impact of abnormal uterine bleeding care in premenopausal patients prior to endometrial malignancy diagnosis. Gynecol Oncol Rep. 2023;50:101292.
doi pubmed - Crosbie E, Morrison J. The emerging epidemic of endometrial cancer: Time to take action. Cochrane Database Syst Rev. 2014;2014(12):ED000095.
doi pubmed - Mittermeier T, Farrant C, Wise MR. Levonorgestrel-releasing intrauterine system for endometrial hyperplasia. Cochrane Database Syst Rev. 2020;9(9):CD012658.
doi pubmed - Bacon JL. Abnormal Uterine Bleeding: Current Classification and Clinical Management. Obstet Gynecol Clin North Am. 2017;44(2):179-193.
doi pubmed - James AH, Kouides PA, Abdul-Kadir R, Edlund M, Federici AB, Halimeh S, Kamphuisen PW, et al. Von Willebrand disease and other bleeding disorders in women: consensus on diagnosis and management from an international expert panel. Am J Obstet Gynecol. 2009;201(1):12.e11-18.
doi pubmed - Ray S, Ray A. Non-surgical interventions for treating heavy menstrual bleeding (menorrhagia) in women with bleeding disorders. Cochrane Database Syst Rev. 2016;11(11):CD010338.
doi pubmed - Zia A, Rajpurkar M. Challenges of diagnosing and managing the adolescent with heavy menstrual bleeding. Thromb Res. 2016;143:91-100.
doi pubmed - Cooper DB, Patel P. Oral Contraceptive Pills. In: StatPearls. Treasure Island (FL). 2024.
pubmed - Campos RR, Baeta T, Silva-Filho A, Rezende SM, Rocha ALL. Use of a levonorgestrel 52-mg intrauterine system in the control of abnormal uterine bleeding in women with inherited bleeding disorders. Contraception. 2020;102(4):254-258.
doi pubmed - Kingman CE, Kadir RA, Lee CA, Economides DL. The use of levonorgestrel-releasing intrauterine system for treatment of menorrhagia in women with inherited bleeding disorders. BJOG. 2004;111(12):1425-1428.
doi pubmed - MacGregor B, Munro MG, Lumsden MA. Therapeutic options for the management of abnormal uterine bleeding. Int J Gynaecol Obstet. 2023;162(Suppl 2):43-57.
doi pubmed - Hickey M, Higham JM, Fraser I. Progestogens with or without oestrogen for irregular uterine bleeding associated with anovulation. Cochrane Database Syst Rev. 2012;2012(9):CD001895.
doi pubmed - Gallos ID, Shehmar M, Thangaratinam S, Papapostolou TK, Coomarasamy A, Gupta JK. Oral progestogens vs levonorgestrel-releasing intrauterine system for endometrial hyperplasia: a systematic review and metaanalysis. Am J Obstet Gynecol. 2010;203(6):547.e541-510.
doi pubmed - Bofill Rodriguez M, Lethaby A, Low C, Cameron IT. Cyclical progestogens for heavy menstrual bleeding. Cochrane Database Syst Rev. 2019;8(8):CD001016.
doi pubmed - Yaaqoub NK. A comparative study between norethisterone progestogens and dydrogesterone in the treatment of dysfunctional uterine bleeding. Current Research in Medicine. 2010;1(1).
- Yasin A, Aziz U. A comparison between the effectiveness of norethisterone and dydrogesterone for treatment of irregular menstrual cycle. Pakistan Journal of Medical and Health Sciences. 2021;15(11):2876-2878.
- Huvinen E, Holopainen E, Heikinheimo O. Norethisterone and its acetate - what's so special about them? BMJ Sex Reprod Health. 2021;47(2):102-109.
doi pubmed - Naib JM, Siddiqui MI, Ajmal W. The role of dydrogesterone in the medical management of 100 cases of dysfunctional uterine bleeding (DUB) above 35 years of age. Journal of Postgraduate Medical Institute. 2011;17(2).
- Tajjamal A. Severity of bleeding is a predictor of quality of life in women with heavy menstrual bleeding under dydrogesterone treatment in a prospective, multicentre, observational study. Gazz Med Ital - Arch Sci Med. 2015;174(9):391-398.
- Trivedi N, Chauhan N, Vaidya V. Effectiveness and safety of dydrogesterone in regularization of menstrual cycle: a post-marketing study. Gynecol Endocrinol. 2016;32(8):667-671.
doi pubmed - Podzolkova N, Tatarchuk T, Doshchanova A, Eshimbetova G, Pexman-Fieth C. Dydrogesterone treatment for menstrual-cycle regularization in routine clinical practice: a multicenter observational study. Gynecol Endocrinol. 2016;32(3):246-249.
doi pubmed - Wang L, Guan HY, Xia HX, Chen XY, Zhang W. Dydrogesterone treatment for menstrual-cycle regularization in abnormal uterine bleeding - ovulation dysfunction patients. World J Clin Cases. 2020;8(15):3259-3266.
doi pubmed - Jones K, Sung S. Anovulatory Bleeding. In: StatPearls. Treasure Island (FL). 2024.
pubmed - Guzick DS, Wing R, Smith D, Berga SL, Winters SJ. Endocrine consequences of weight loss in obese, hyperandrogenic, anovulatory women. Fertil Steril. 1994;61(4):598-604.
pubmed - Bofill Rodriguez M, Lethaby A, Jordan V. Progestogen-releasing intrauterine systems for heavy menstrual bleeding. Cochrane Database Syst Rev. 2020;6(6):CD002126.
doi pubmed - Kaunitz AM, Meredith S, Inki P, Kubba A, Sanchez-Ramos L. Levonorgestrel-releasing intrauterine system and endometrial ablation in heavy menstrual bleeding: a systematic review and meta-analysis. Obstet Gynecol. 2009;113(5):1104-1116.
doi pubmed - Bardawil E, et al. Endometrial ablation - current evidence for patient optimization and long-term outcomes. Current Obstetrics and Gynecology Reports, 2018;7(2):66-73.
- Ali M, A RS, Al Hendy A. Elagolix in the treatment of heavy menstrual bleeding associated with uterine fibroids in premenopausal women. Expert Rev Clin Pharmacol. 2021;14(4):427-437.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Gynecology and Obstetrics is published by Elmer Press Inc.