The clinician should obtain a detailed history from a patient who presented with complaints related to menstruation [15, 16]:
1) Menstrual history, including age at menarche, last menstrual period, and intermenstrual and postcoital bleeding. Additionally, the frequency, regularity, duration, and the volume of flow of menses should be recorded:
a) Frequency can be described as frequent (less than 24 days), normal (24 to 38 days), or infrequent (greater than 38 days).
b) Regularity can be described as absent, regular (with a variation of ± 2 to 7 days), or irregular (variation greater than 20 days).
c) The duration can be described as prolonged (greater than 8 days), normal (approximately 4 to 8 days), or shortened (less than 4 days).
d) The volume of flow can be described as heavy (greater than 80 mL), normal (5 to 80 mL), or light (less than 5 mL of blood loss)a.
2) Sexual and reproductive history: obstetrical history, including the number of pregnancies and mode of delivery, fertility desire and subfertility, current contraception, possibility of pregnancy, history of STIs, history of Pap smear, history of vaccination, and any previous diagnostic management (i.e., endometrial biopsy, etc.).
3) Systemic symptoms such as any history of weight loss, pain, discharge, bowel or bladder symptoms, symptoms or history of bleeding disorders, symptoms or history of endocrine disorders.
4) Symptoms of anemia: headache, palpitations, shortness of breath, dizziness, fatigue, and pica.
5) Associated symptoms: fever, chills, increasing abdominal girth, pelvic pressure or pain, bowel or bladder dysfunction, vaginal discharge, or odor.
6) Symptoms associated with a systemic cause for AUB: overweight, obesity, PCOS, hypothyroidism, hyperprolactinemia, hypothalamic or adrenal disorder.
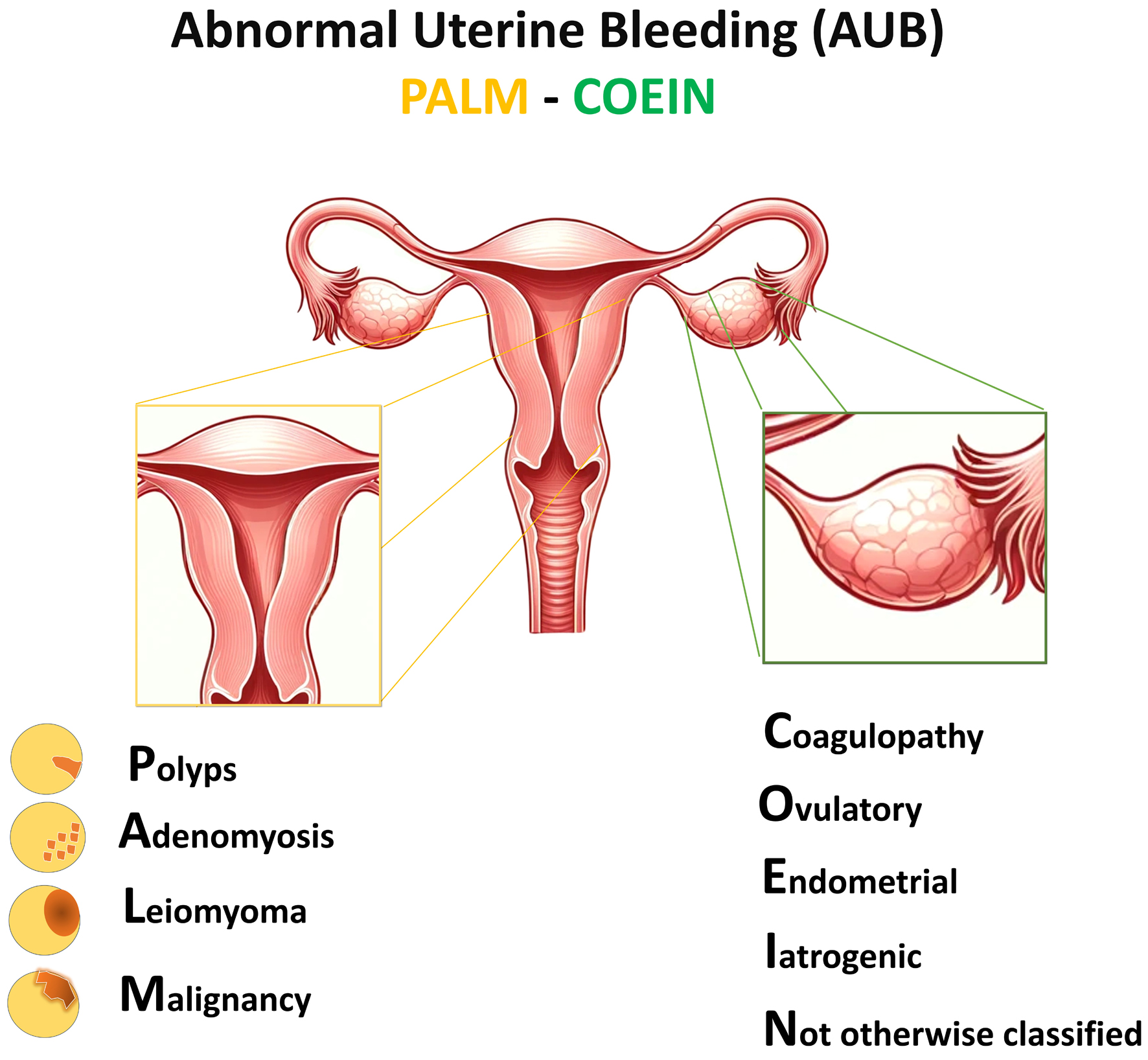
7) Chronic medical illness: inherited bleeding disorders (coagulopathy, blood dyscrasias, and platelet functional disorders), systemic lupus erythematosus or other connective tissue diseases, liver disease, renal disease, and cardiovascular disease.
8) Current medication intake: hormonal contraceptives, anticoagulants, SSRIs, antipsychotics, tamoxifen, and herbals (e.g., Ginseng).
9) Family history including questions concerning coagulopathies, malignancy, and endocrine disorders.
10) Social history including tobacco, alcohol, and drug uses; occupation; the impact of symptoms on quality of life.
11) Surgical history. |