| Vaginal hysterectomy | | | | | | |
Ahmed et al [9]
Mean ± SD | Intervention: LigaSure (n = 20)
Control: Sutures (n = 20) | Intervention: 315 ± 191.3 mL
Control: 592.5 ± 296.2 mLc | Intervention:
53.95 ± 6.94 min
Control:
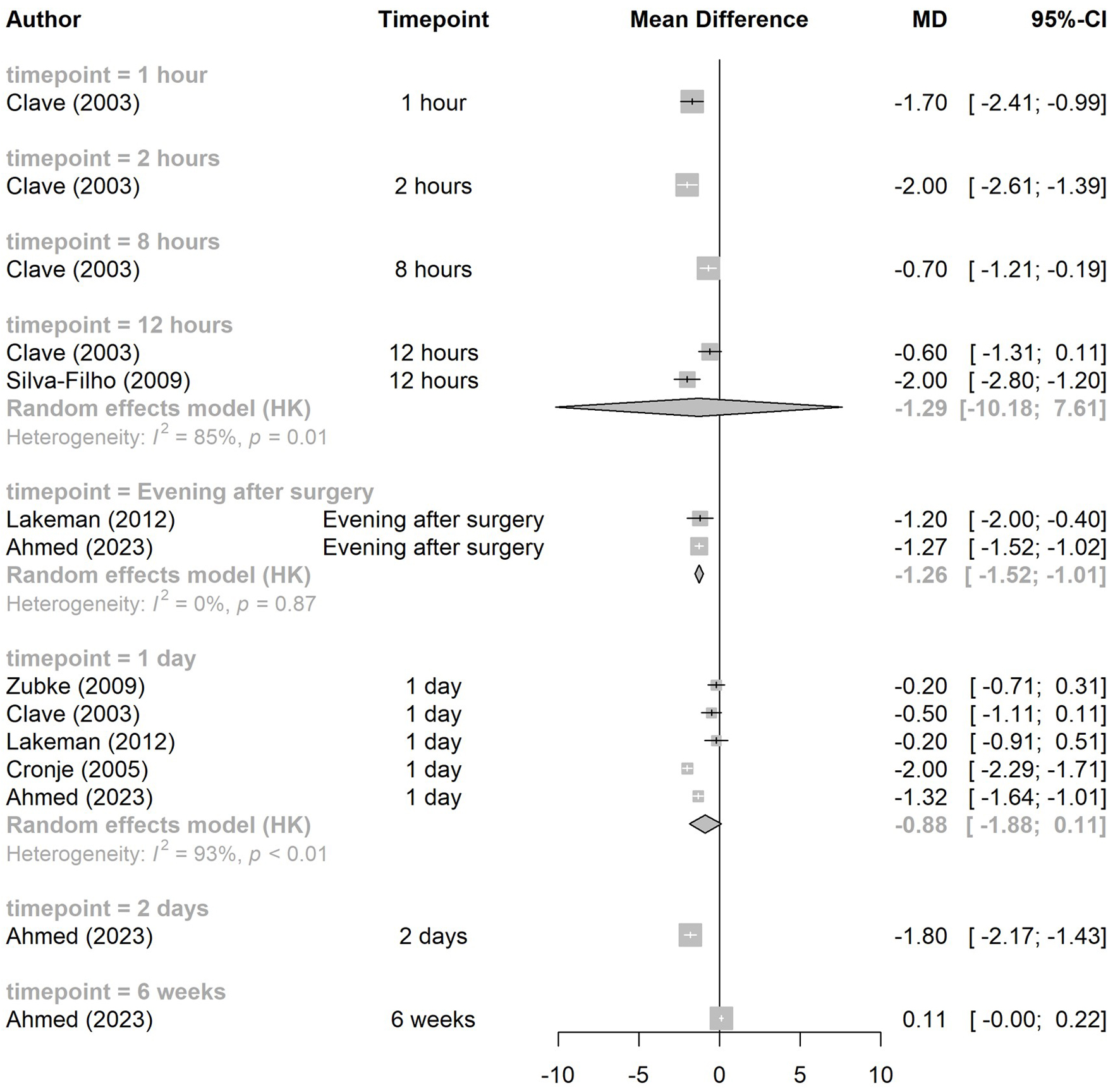
62.90 ± 7.28 minc | NR | Evening after surgery:
Intervention: 54.50 ± 4.47;
Control: 67.20 ± 3.55c
1 day:
Intervention: 46.70 ± 5.68;
Control: 59.95 ± 4.52c
2 days:
Intervention: 35.50 ± 6.82;
Control: 53.50 ± 5.08c
6 weeks:
Intervention: 11.20 ± 2.12;
Control: 10.10 ± 1.48a | Intervention: 0
Control: 1a |
Ray et al [10]
Median (interquartile range) | Intervention: LigaSure (n = 48)
Control: Sutures (n = 47) | Intervention: 100 (50 to 200) mL
Control: 100 (50 to 150) mLa | Intervention:
40.5 (29.75 to 52) min
Control:
38 (33 to 46) mina | “4 vs 4.83 h”d
It is not entirely clear within the article which value is for which group. It is assumed the first value is for the intervention group. | 0 day:
Intervention, n = 45: 49 (25 to 75);
Control, n = 46: 50.5 (32.25 to 66.5)a
1 day:
Intervention, n = 42: 40.5 (21.2 to 56.75);
Control, n = 44: 42 (20.5 to 64)a
3 days:
Intervention, n = 42: 30.5 (13.75 to 48);
Control, n = 44: 40 (13.75 to 67)a
5 days:
Intervention, n = 42: 16.5 (5.25 to 33.75);
Control, n = 44: 23 (4 to 40.75)a
2 weeks:
Intervention, n = 35: 2 (0 to 13.5);
Control, n = 38: 4 (1 to 10)a | Intervention: 0
Control: 0d |
| Laparoscopic hysterectomy | | | | | | |
Ashraf et al [24]
Mean ± SD | Intervention: LigaSure (n = 20)
Control: UltraCision harmonic shears (n = 20) | NR | Intervention:
64.15 ± 12.02 min
Control:
138.25 ± 23.41 minc | Intervention: 1.65 ± 0.58 days
Control: 2.00 ± 1.52 daysa | NR | NR |
Batra et al [8]
Mean ± SD | Intervention: LigaSure (n = 60)
Control: Conventional EBVS (n = 60) | Intervention: 141.67 ± 101.75 mL
Control: 145 ± 84.7 mLa | Primary OT:
Intervention:
74.388 ± 11.84 min;
Control:
97.0319 ± 13.425 minc
Total OT:
Intervention:
136.37 ± 14.35 min;
Control:
142.50 (SD not reported) minc | Intervention: 2.32 ± 0.56 days
Control: 2.54 ± 0.988 daysa | NR | NR |
Hasabe et al [25]
Average | Intervention: LigaSure (n = 30)
Controls: harmonic scalpel (n = 30), bipolar shears (n = 30) | NR | Intervention: 54.36 min
Harmonic scalpel: 68.25 min
Bipolar shears: 59.34 mind | Intervention: 1.35 days
Harmonic scalpel: 1.84 days
Bipolar shears: 1.60 daysd | NR | NR |
Janssen et al [22]
Mean ± SD | Intervention: Ligasure (n = 66)
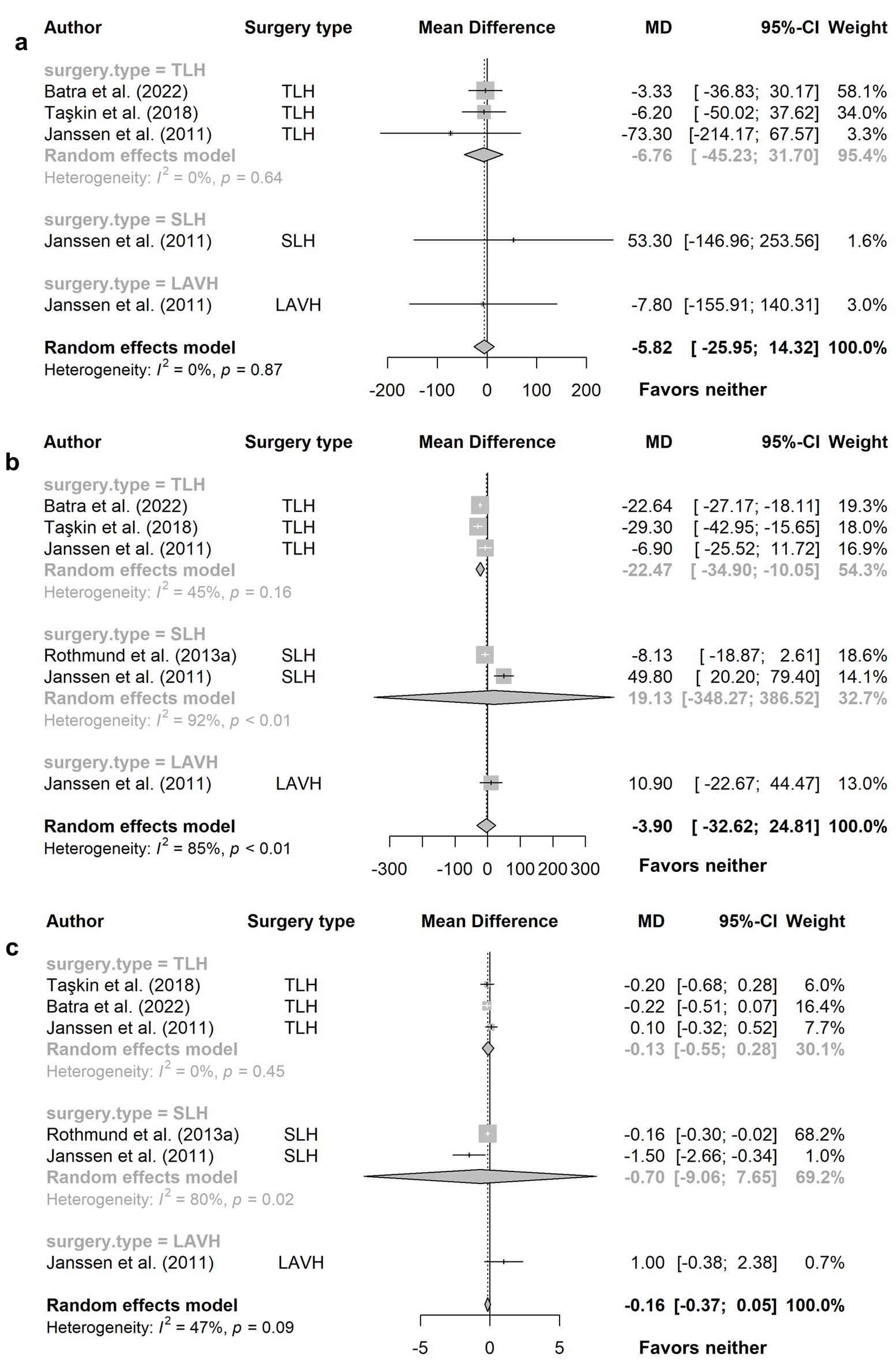
Control: conventional EBVS (n = 65) | All LH:
Intervention: 234.1 ± 263 mL;
Control: 273.1 ± 329 mLa
TLH:
Intervention: 232.6 ± 286 mL;
Control: 305.9 ± 375 mLd
LAVH:
Intervention: 212.2 ± 133 mL;
Control: 220.0 ± 212 mLd
SLH:
Intervention: 255.8 ± 257 mL;
Control: 202.5 ± 233 mLd | OT to detachment of uterus
All LH:
Intervention: 97.6 ± 31.4 min; Control: 91.8 ± 35.4 mina
TLH:
Intervention: 92.1 ± 33.8 min; Control: 98.1 ± 38.5 mind
LAVH:
Intervention: 105.5 ± 25.3 min; Control: 82.71 ± 28.7 mind
SLH:
Intervention: 111.5 ± 21.1 min; Control: 76.4 ± 22.8 mind
Total OT
All LH:
Intervention: 148.2 ± 43.6 min; Control: 142.1 ± 46.1 mina
TLH:
Intervention: 140.3 ± 39.0 min; Control: 147.2 ± 48.7 mind
LAVH:
Intervention: 130.9 ± 35.5 min; Control: 120.0 ± 42.9 mind
SLH:
Intervention: 190.8 ± 42.5 min; Control: 141.0 ± 29.2 mind | All LH:
Intervention: 2.9 ± 1.3 days;
Control: 2.9 ± 1.0 daysa
TLH:
Intervention: 2.9 ± 1.1 days;
Control: 2.8 ± 0.9 daysd
LAVH:
Intervention: 3.8 ± 2.0 days;
Control: 2.8 ± 0.8 daysd
SLH:
Intervention: 2.1 ± 0.8 days;
Control: 3.6 ± 1.8 daysd | NR | NR |
| Rothmund et al [26] | Intervention: EnSeal (n = 80)
Control: conventional EBVS (n = 80) | Less than 50 mL blood loss (n):
Intervention: 72; Control: 62b
50 to 100 mL blood loss (n):
Intervention: 8; Control: 18c | Total OT (mean ± SD):
Intervention: 78.18 ± 33.96 min; Control: 86.31 ± 35.35 minb
T1:
Intervention: 15.10 ± 5.51 min; Control: 16.21 ± 5.53 mina
T2:
Intervention: 24.90 ± 14.80 min; Control: 36.23 ± 25.44 minc
T3:
Intervention: 38.00 ± 22.25 min; Control: 33.86 ± 14.12 mina | Intervention: 2.01 ± 0.44 days
Control: 2.17 ± 0.47 daysb | Day 1:
Intervention: 3.44 ± 1.62; Control: 3.18 ± 1.71a
Day 2: (n = 154)
Intervention (77): 2.03 ± 1.49; Control (77): 1.96 ± 1.38a
Day 3: (n = 25)
Intervention (8): 2.13 ± 1.26; Control (17): 1.59 ± 1.58a | Intervention: 0
Control: 0d |
Rothmund et al [27]
Mean ± SD | Intervention: BiCision
Control: UltraCision harmonic scalpel
n = 30 (self-controlled trial) | Overall intraoperative blood loss score:
Intervention: 1.07 ± 0.25;
Control: 1.63 ± 0.49c | Intervention: 8.8 ± 1.8 min
Control: 8.3 ± 1.9 mina | NR | NR | Intervention: 0
Control: 0d |
Taşkin et al [23]
Mean ± SD | Intervention: LigaSure (n = 34)
Control: conventional EBVS (n = 34) | Intervention: 176.1 ± 78.2 mL
Control: 182.3 ± 104.3 mLa | Intervention: 134.2 ± 29.7 min
Control: 163.5 ± 27.7 minc | Intervention: 1.9 ± 0.9 days
Control: 2.1 ± 1.1 daysa | 8 h:
Intervention: 3.3 ± 1.1;
Control: 3.6 ± 0.9a
24 h:
Intervention: 2.1 ± 0.8;
Control: 2.1 ± 0.9a | Intervention: 2
Control: 4a |
| Abdominal hysterectomy | | | | | | |
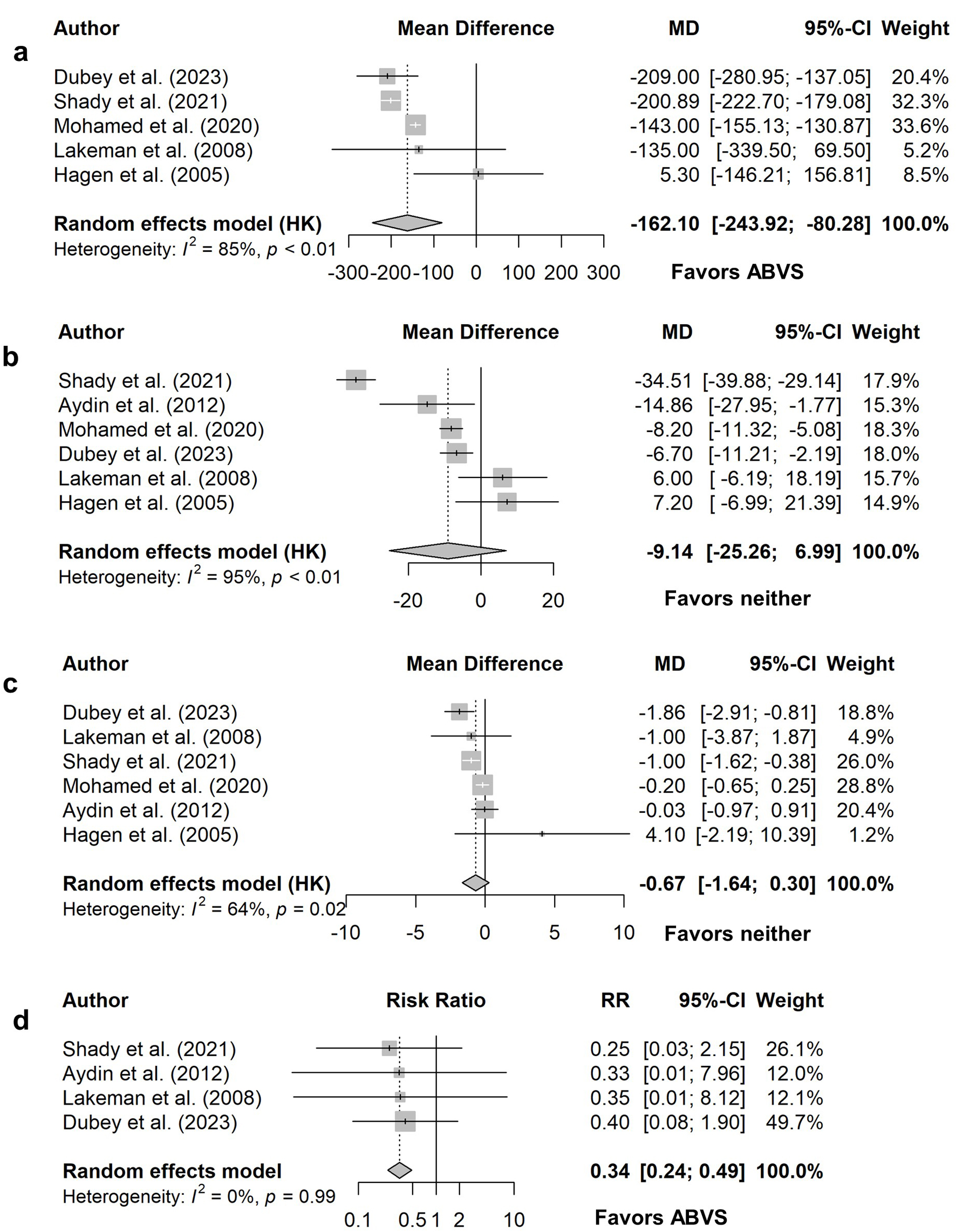
Aydin et al [28]
Mean ± SD | Intervention: LigaSure (n = 44)
Control: Sutures (n = 44) | NR | Intervention: 109.91 ± 26.55 min
Control: 124.77 ± 35.51 minb | Intervention: 5.92 ± 2.63 days
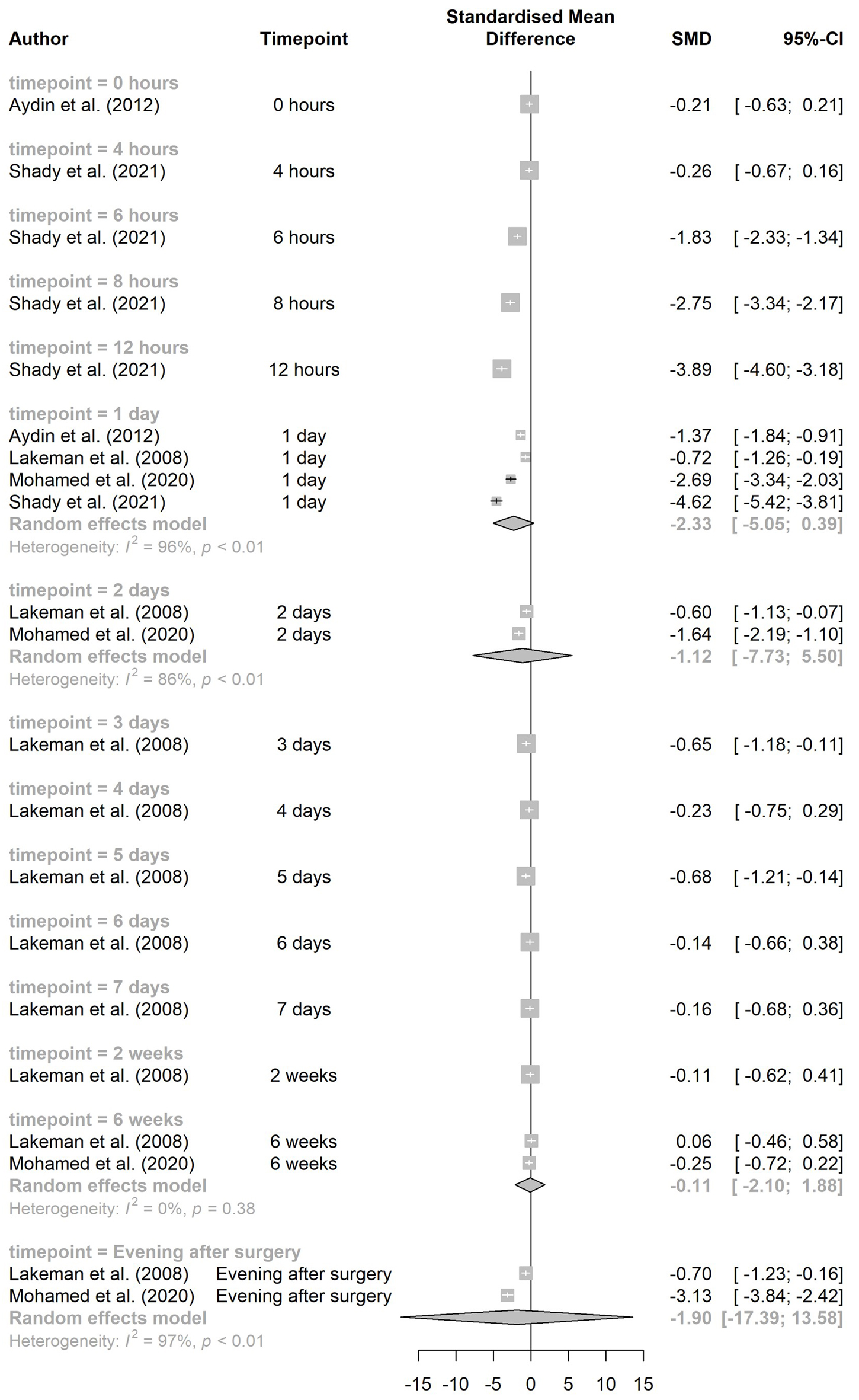
Control: 5.95 ± 1.82 daysa | 0 h:
Intervention: 6.02 ± 1.17;
Control: 6.25 ± 1.01a
24 h:
Intervention: 1.07 ± 0.66;
Control: 1.93 ± 0.58a | Intervention: 0
Control: 1d |
Dubey et al [29]
Mean ± SD | Intervention: LigaSure (n = 30)
Control: Sutures (n = 30) | Intervention: 111 ± 53.31 mL
Control: 320 ± 193.90 mLc | Intervention: 26.97 ± 9.08 min
Control: 33.67 ± 8.77 minc | Intervention: 3.57 days
Control: 5.43 daysc
(SD NR) | 1 day:
Intervention: mode 6;
Control: mode 8d
2 days:
Intervention: mode 3;
Control: mode 6d
3 days:
Intervention: mode 2;
Control: mode 3d | Intervention: 2
Control: 5d |
Hagen et al [30]
Mean | Intervention: LigaSure (n = 15)
Control: Sutures (n = 15) | Intervention: 303 mL
Control: 298 mLd | Intervention: 61.7 min
Control: 54.5 mind | Intervention: 10 days
Control: 6 daysd | NR | NR |
Lakeman et al [31]
Median (range) | Intervention: LigaSure (n = 28)
Control: Sutures (n = 29) | Intervention: 200 (33 to 1,500) mL
Control: 335 (70 to 1,750) mLa | Intervention: 69 (29 to 130) min
Control: 63 (38 to 124) mina | Intervention: 4 (2 to 32) days
Control: 5 (3 to 11) daysa | Evening after surgery (mean (SE)):
Intervention: 52 (5); Control: 69 (4)c
1 day (mean (SE)):
Intervention: 47 (5); Control: 63 (3)d
2 days (mean (SE)):
Intervention: 36 (4); Control: 49 (4)d
3 days (mean (SE)):
Intervention: 27 (4); Control: 41 (4)d
4 days (mean (SE)):
Intervention: 28 (4); Control: 33 (4)a
5 days (mean (SE)):
Intervention: 20 (3); Control: 31 (4)d
6 days (mean (SE)):
Intervention: 24 (4); Control: 27 (4)d
7 days (mean (SE)):
Intervention: 18 (3); Control: 21 (4)d
2 weeks (mean (SE)):
Intervention: 14 (4); Control: 16 (3)a
6 weeks (mean (SE)):
Intervention: 11 (3); Control: 10 (3)d | Intervention: 0
Control: 1d |
Mohamed et al [32]
Mean ± SD | Intervention: LigaSure (n = 35)
Control: Sutures (n = 35) | Intervention: 142.7 ± 23.1 mL
Control: 285.7 ± 28.4 mLc | Intervention: 54.9 ± 6.7 min
Control: 63.1 ± 6.6 minc | Intervention: 0.80 ± 0.93 days
Control: 1.0 ± 1.0 daysa | Evening after surgery:
Intervention: 54.3 ± 4.8; Control: 68.3 ± 4.0c
1 day:
Intervention: 46.1 ± 4.7; Control: 60.3 ± 5.7c
2 days:
Intervention: 34.1 ± 5.7; Control: 43.0 ± 5.0c
6 weeks:
Intervention: 10.6 ± 2.1; Control: 11.1 ± 1.8a | NR |
Shady et al [33]
Mean ± SD | Intervention: LigaSure (n = 45)
Control: Sutures (n = 45) | Intraoperative:
Intervention: 270.44 ± 51.39 mL;
Control: 471.33 ± 54.13 mLc
Postoperative:
Intervention: 69.78 ± 14.998 mL;
Control: 108.00 ± 26.68 mLc
Total:
Intervention: 340.22 ± 56.67 mL;
Control: 579.11 ± 70.61 mLc | Intervention: 61.78 ± 15.71 min
Control: 96.29 ± 9.51 minc | Intervention: 2 (1 to 7) days
Control: 3 (2 to 8) daysc
Median (range) | 4 h:
Intervention: 8.49 ± 1.06; Control: 8.76 ± 1.00a
6 h:
Intervention: 6.62 ± 0.96; Control: 8.49 ± 1.06c
8 h:
Intervention: 4.80 ± 0.87; Control: 7.33 ± 0.95c
12 h:
Intervention: 3.71 ± 0.76; Control: 7.02 ± 0.92c
24 h:
Intervention: 1.67 ± 0.798; Control: 5.73 ± 0.94c | Intervention: 1
Control: 4a |