| Journal of Clinical Gynecology and Obstetrics, ISSN 1927-1271 print, 1927-128X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Gynecol Obstet and Elmer Press Inc |
| Journal website https://jcgo.elmerpub.com |
Case Report
Volume 000, Number 000, October 2025, pages 000-000
A Case of Mucous Membrane Pemphigoid Masquerading as Lichen Planus
Sierra R. Parkinsona, c, Sabah Osmanib, Sarah B. Corleyb
aMD Program, Department of Medical Education, School of Medicine, University of North Carolina at Chapel Hill, Chapel Hill, NC, USA
bDivision of Vulvar Dermatology, Department of Dermatology, School of Medicine, University of North Carolina at Chapel Hill, Chapel Hill, NC, USA
cCorresponding Author: Sierra Parkinson, University of North Carolina at Chapel Hill School of Medicine, Chapel Hill, NC 27599, USA
Manuscript submitted September 23, 2025, accepted October 4, 2025, published online October 10, 2025
Short title: Genital Mucous Membrane Pemphigoid
doi: https://doi.org/10.14740/jcgo1545
| Abstract | ▴Top |
Mucous membrane pemphigoid (MMP) is a rare, autoimmune blistering disease that affects mucosal surfaces and can mimic other inflammatory dermatoses such as erosive lichen planus (LP), lichen sclerosus, and pemphigus vulgaris. Diagnosis is challenging due to overlapping clinical and histopathological features, especially when hematoxylin and eosin (H&E) staining reveals nonspecific lichenoid changes. We report the case of a 79-year-old woman with a 2-year history of therapy-resistant vulvar erosions, pruritus, and pain. Initial physical exam performed by gynecology noted a focal erosion of the introitus. A vulvar biopsy showed lichenoid infiltrate with scattered eosinophils. She was initially treated with clobetasol 0.05% ointment and tacrolimus 0.1% ointment for presumed LP, without clinical improvement. The patient had also developed erosions of the oral and nasal cavities, in addition to conjunctival injection and symblepharon, prompting a biopsy of the left conjunctiva by her ophthalmologist. Direct immunofluorescence (DIF) of the conjunctiva showed linear deposits of IgG, IgA, and C3 at the basement membrane zone, consistent with MMP. Upon referral to our vulvar dermatology clinic, she was receiving rituximab infusions for her MMP and applying clobetasol 0.05% ointment to her nasal, oral, and genital ulcers. Despite improvement in the nasal and oral ulcers, vulvovaginal pruritus and pain persisted. Exam in our office was notable for well demarcated pink patches on the bilateral medial labia majora with erosions beginning in the introitus and extending into the vagina with surrounding white hyperkeratotic epithelium. Architectural changes were seen including labial agglutination, partial clitoral phimosis, and introital stenosis. Given vaginal and introital involvement, she was started on nightly hydrocortisone 25 mg vaginal suppositories and halobetasol 0.05% ointment to be applied to the labia and introitus. At follow-up, the patient reported significant improvement in pain with minimal pruritus and notable improvement of the erosions and erythema. This case uniquely contributes to the literature by highlighting the diagnostic challenges of vulvar MMP and emphasizing the importance of maintaining a high clinical suspicion for MMP when lichenoid features are present on H&E, especially in the setting of extra-genital mucosal erosions. Early recognition and diagnostic confirmation with DIF are paramount for ensuring timely treatment initiation and prevention of irreversible disease progression.
Keywords: Mucous membrane pemphigoid; Vulvar pemphigoid; Vulvar lichen planus; Mucocutaneous disease
| Introduction | ▴Top |
Mucous membrane pemphigoid (MMP) is a rare, chronic autoimmune blistering disease that predominantly affects mucosal surfaces, leading to painful erosions and progressive scarring. While the oral and ocular mucosa are most commonly involved, the vulvovaginal region can also be affected, often mimicking other inflammatory dermatoses such as erosive lichen planus, lichen sclerosus, and pemphigus vulgaris [1]. This overlap in clinical and histopathological features poses a diagnostic challenge, particularly when hematoxylin and eosin (H&E) staining reveals nonspecific lichenoid patterns.
In this report, we present a diagnostically complex case of vulvovaginal MMP in an elderly woman, initially misdiagnosed as lichen planus based on histopathology showing a lichenoid infiltrate. Additionally, despite partial improvement with systemic rituximab and topical corticosteroids, her genital symptoms persisted until the initiation of hydrocortisone vaginal suppositories. This case highlights the importance of maintaining a broad differential diagnosis for chronic vulvar erosions and highlights the critical role of DIF in identifying MMP and the use of vaginal steroid suppositories for treatment.
| Case Report | ▴Top |
Investigations
A 79-year-old woman with a history of end-stage renal disease on hemodialysis, and chronic hepatitis C was referred to our dermatology clinic for evaluation of a 2-year history of vulvar itching, burning, and pain. She was initially evaluated by her gynecologist, who noted a focal 2 × 3 cm erosion of the introitus. A vulvar biopsy at that time stained with H&E revealed a lichenoid infiltrate with scattered eosinophils, and the diagnosis of vulvar lichen planus was made. She was treated with clobetasol 0.05% ointment twice daily for 4 weeks and tacrolimus 0.1% ointment twice daily for another 6 weeks, neither of which provided clinical improvement.
The patient concurrently developed erosions of the oral and nasal cavities, as well as conjunctival injection and the formation of symblepharon. These findings prompted her ophthalmologist to perform a biopsy of the left conjunctiva. DIF of the conjunctive demonstrated linear deposits of IgG, IgA, and C3 at the basement membrane zone, consistent with MMP. She was subsequently referred to an autoimmune dermatologist for systemic management and began receiving rituximab infusions.
When the patient presented to our vulvar dermatology clinic, she had been receiving rituximab infusions and applying clobetasol 0.05% ointment to her nasal, oral, and genital ulcers. Although her oral and nasal mucosal ulcers had improved, she continued to experience persistent vulvovaginal pruritus and pain. Physical examination in our clinic revealed well demarcated pink patches on the bilateral medial labia majora with erosions beginning in the introitus and extending into the vagina with surrounding white hyperkeratotic epithelium. Architectural changes were seen including labial agglutination, partial clitoral phimosis, and introital stenosis (Fig. 1).
 Click for large image | Figure 1. Well demarcated pink patches on the bilateral medial labia majora (green arrows) with erosions beginning in the introitus and extending into the vagina (white arrow) with surrounding white hyperkeratotic epithelium. The mass of the labia minora was partially reduced with agglutination laterally to the labia majora along with partial retraction of the clitoral hood (red arrow) and significant narrowing of the introitus aperture and minimal visibility of the urethral meatus. |
Diagnosis
The diagnosis of genital MMP was ultimately made based on a combination of clinical presentation and DIF findings. During the early stages of evaluation, a vulvar biopsy revealed a lichenoid infiltrate with scattered eosinophils, leading to an initial diagnosis of vulvar lichen planus. This led to treatment with topical corticosteroids and calcineurin inhibitors, which failed to yield clinical improvement.
Given involvement of the ocular mucosa, additional evaluation by an ophthalmologist was undertaken. A biopsy of the left conjunctiva with direct immunofluorescence (DIF) revealed linear deposition of IgG, IgA, and C3 along the basement membrane zone, confirming the diagnosis of MMP. This diagnosis explained her multifocal mucosal involvement and poor response to therapies directed at presumed lichen planus.
The initial diagnosis was complicated by the nonspecific lichenoid findings on H&E stain. The evolution of mucosal erosions and scarring in multiple sites, and ultimately evaluation with DIF, clarified the diagnosis. A timeline of the patient’s symptom onset, diagnostic evaluations, and therapeutic interventions is summarized in Figure 2. Prognostically, MMP is a chronic autoimmune blistering disease that can lead to significant scarring, functional impairment, and even irreversible blindness [1].
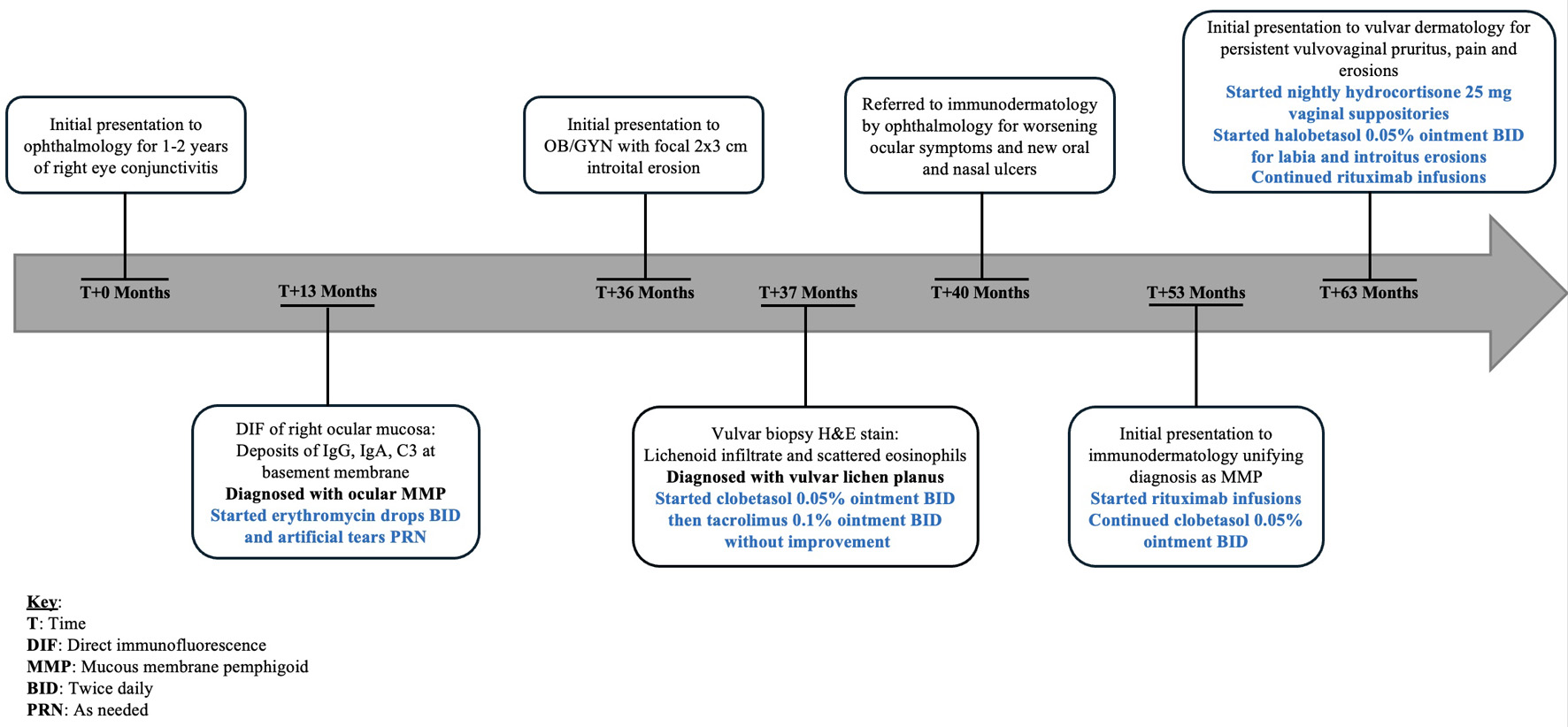 Click for large image | Figure 2. Timeline of the patient’s symptom onset, diagnostic evaluations, and treatment interventions. |
Treatment
Upon diagnosis of MMP with multisite mucosal involvement, the patient was initiated on rituximab infusions by an autoimmune dermatologist for systemic immunosuppression. Concurrently, she was applying clobetasol 0.05% ointment to her oral, nasal, and genital ulcers. While some improvement was observed in the nasal and oral mucosae, her vulvovaginal symptoms remained refractory to this regimen.
At our vulvar dermatology clinic, a more targeted approach was implemented to address the vaginal and introital erosions with the initiation of nightly hydrocortisone 25 mg vaginal suppositories and halobetasol 0.05% ointment for application to the labia and introitus. These interventions were selected to maximize anti-inflammatory effects in the vulvovaginal region and to facilitate application of the medication in an anatomically difficult to reach area.
Follow-up and outcomes
At follow-up, the patient reported significant improvement in vulvovaginal pain and a marked reduction in pruritus with the initiation of vaginal hydrocortisone 25 mg suppositories. Given symptom control, the frequency of hydrocortisone suppositories was reduced from nightly to twice a week with continued use of halobetasol 0.05% ointment nightly. Clinically, there was notable improvement in the appearance of erosions and surrounding erythema. The architectural changes, including agglutination, urethral meatus visibility, and introital narrowing, remained stable, with no progression.
The patient demonstrated adherence to the prescribed therapies, and there were no reported adverse events or side effects from the hydrocortisone suppositories or halobetasol ointment. Tolerability was adequate, and her improvement was confirmed by both subjective symptom relief and objective clinical findings on examination. No further mucosal involvement was noted, and ongoing monitoring was planned to assess for long-term control and maintenance of disease remission.
| Discussion | ▴Top |
MMP is a rare autoimmune disease that primarily affects mucosal surfaces and can present as painful subepidermal blisters, often progressing to chronic erosions and ulcers [1]. Disease is thought to be caused by circulating antibodies that target the basement membrane zone with common antigens including laminin 332 (associated with malignancy), β4 subunit (ocular MMP), and BP180 (collagen XVII) [1]. The healing phase is often associated with scarring, leading to structural changes. MMP can involve any mucous membrane with layered squamous cell epithelium, most commonly the oral mucosa and conjunctiva, though the nasal cavity, larynx, esophagus, and vulvovaginal mucosa may also be affected [1].
Since involvement of the vulva in MMP may result in scarring architectural changes such as stenosis of the introitus and urethral meatus, agglutination of the labia minora, and clitoral phimosis, distinguishing it from other vulvar dermatoses such as erosive LP, lichen sclerosus, and pemphigus vulgaris, can be challenging [2]. Although all these disorders may respond to topical ultrapotent corticosteroids, this does not preclude the need for a correct diagnosis because each may affect different organ systems and have different prognoses.
A recent study investigating the frequency of lichenoid features in MMP found that 22% of DIF-confirmed MMP cases exhibited lichenoid features on H&E stain. Clinically, 11 of the 18 cases were initially suspected to be oral LP [3]. These findings emphasize that although lichenoid features are common in mucosal inflammatory conditions, rarer diagnoses, like MMP, should remain on the differential. Genital MMP can present with a range of clinical and histopathological findings, including lichenoid features [4], and should be considered in patients with chronic vulvar pain and/or pruritus in the setting of introital erosions, particularly when accompanied by extra-genital manifestations such as ocular, nasal, or oral ulcers [4].
If MMP is suspected, clinicians should know that H&E is often nonspecific and overlaps with other conditions, and the gold standard for diagnosis is DIF showing linear deposits of IgG, IgA, and C3 at the basement membrane zone. As seen in this case report, DIF was crucial to diagnosis and systemic treatment initiation of MMP.
Guidelines for the treatment of MMP recommend the use of aggressive immunosuppressants or immunomodulators to prevent progression and serious complications. These range from dapsone and tetracyclines with nicotinamide for mild disease to mycophenolate mofetil, intravenous immunoglobulin (IVIG), and rituximab for more severe disease. Additionally, systemic and intralesional steroids may be helpful [1]. For genital involvement, potent topical steroid use once daily is the standard recommendation, with calcineurin inhibitors considered as an alternative [1]. The addition of vaginal suppositories, such as hydrocortisone 25 mg, may serve as an additional therapeutic option for the intravaginal and introital manifestations of MMP, as seen in our patient. Vaginal suppositories are especially useful for patients who have difficulty applying medication to the introitus, as in this case.
Although cases of genital mucous membrane pemphigoid have been reported in the literature, this report highlights a unique presentation of genital MMP masquerading as LP and reinforces the importance for clinicians to maintain a high index of suspicion for MMP when lichenoid features are present on H&E, especially in the setting of extra-genital mucosal erosions. Early recognition and diagnosis with DIF are paramount in ensuring timely detection and treatment to prevent disease progression.
Learning points
This case highlights the diagnostic challenges of MMP, particularly when it presents with lichenoid features that mimic more common inflammatory dermatoses like lichen planus. In patients with chronic, treatment-resistant vulvar erosions, especially when accompanied by mucosal involvement at other sites such as the oral, nasal, or ocular mucosa, clinicians should maintain a high index of suspicion for MMP. Histopathology with H&E staining may be nonspecific, and definitive diagnosis often requires DIF showing linear IgG, IgA, and C3 deposition at the basement membrane. Early recognition and accurate diagnosis are critical to initiate appropriate systemic and localized immunosuppressive therapy and prevent irreversible scarring and structural damage.
Acknowledgments
The authors thank the Department of Dermatology at the University of North Carolina at Chapel Hill School of Medicine.
Financial Disclosure
This study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of Interest
None to declare.
Informed Consent
The patient of the present case provided written informed consent. We confirm the ethical approval of the case report.
Author Contributions
Sarah Corley observed the patient and performed medical treatment. Sierra Parkinson drafted the manuscript. Sierra Parkinson, Sabah Osmani, and Sarah Corley reviewed and edited the manuscript. All authors have approved the final article for journal publication.
Data Availability
Data sharing is not applicable to this article as no new data were created or analyzed in this study.
Abbreviations
DIF: direct immunofluorescence; H&E: hematoxylin and eosin; LP: lichen planus; MMP: mucous membrane pemphigoid
| References | ▴Top |
- Hofmann SC, Gunther C, Bockle BC, Didona D, Ehrchen J, Gaskins M, Geerling G, et al. S2k Guideline for the diagnosis and treatment of mucous membrane pemphigoid. J Dtsch Dermatol Ges. 2022;20(11):1530-1550.
doi pubmed - Simonetta C, Burns EK, Guo MA. Vulvar dermatoses: a review and update. Mo Med. 2015;112(4):301-307.
pubmed - McAlpine SG, Googe PB, Culton DA. The frequency of lichenoid features in mucous membrane pemphigoid: A retrospective review of the histopathology. JAAD Int. 2024;17:17-18.
doi pubmed - Rashid H, Oldhoff JM, Esajas M, Diercks GFH, Pas HH, Bolling MC, Horvath B. Juvenile and adult vulvar pemphigoid, an under recognized entity: case series of fourteen patients. JAAD Case Rep. 2021;13:75-80.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Gynecology and Obstetrics is published by Elmer Press Inc.