| Journal of Clinical Gynecology and Obstetrics, ISSN 1927-1271 print, 1927-128X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Gynecol Obstet and Elmer Press Inc |
| Journal website https://jcgo.elmerpub.com |
Short Communication
Volume 000, Number 000, October 2025, pages 000-000
Intrapartum Terbutaline Use and Cesarean Delivery for Labor Dystocia
Cecilia B. Leggetta, e, Lisa Levineb, Melissa Wongc, Jennifer A. McCoyd
aDivision of Maternal Fetal Medicine, Department of Obstetrics and Gynecology, Stanford University School of Medicine, Palo Alto, CA, USA
bDivision of Maternal Fetal Medicine, Department of Obstetrics and Gynecology, University of Pennsylvania, Philadelphia, PA, USA
cDivision of Maternal Fetal Medicine, Department of Obstetrics and Gynecology, Cedars-Sinai Medical Center, Los Angeles, CA, USA
dDivision of Maternal Fetal Medicine, Department of Obstetrics and Gynecology, Dartmouth Geisel School of Medicine, Lebanon, NH, USA
eCorresponding Author: Cecilia B. Leggett, Division of Maternal Fetal Medicine, Department of Obstetrics and Gynecology, Stanford University, Palo Alto, CA, USA
Manuscript submitted July 1, 2025, accepted September 19, 2025, published online October 10, 2025
Short title: Intrapartum Terbutaline Use and Labor Dystocia
doi: https://doi.org/10.14740/jcgo1527
| Abstract | ▴Top |
Background: Terbutaline, a β2-adrenergic agonist used to inhibit uterine contractions, is often used to treat fetal heart rate abnormalities, but whether its use increases the risk of labor dystocia remains understudied. Therefore, we sought to assess the association between intrapartum terbutaline use and cesarean delivery (CD) for labor dystocia.
Methods: We performed a secondary analysis of a single-center prospective cohort study of patients undergoing induction of labor (IOL) at an urban academic hospital from 2013 to 2015. Participants were singleton, full term with intact membranes, and Bishop score of ≤ 6 and dilation ≤ 2 cm undergoing IOL for any indication. Patients with prior CD were excluded. Patients who received terbutaline at any time during their IOL were compared to patients who did not receive terbutaline. The primary outcome was CD due to labor dystocia (defined as failed IOL, arrest of dilation, or arrest of descent).
Results: Of 844 patients, 161 (19%) received terbutaline and 683 (81%) did not. Though the overall rate of CD was higher in the terbutaline group (51% exposed vs. 24% unexposed, P < 0.001), this was primarily driven by CD for fetal distress (26% exposed vs. 4% unexposed, P < 0.001). There was no difference in CD for labor dystocia (24.8% exposed vs. 19.5% unexposed, P = 0.13). Latent phase of labor was longer in the terbutaline group (11.8 h exposed vs. 10.4 h unexposed, P = 0.02), whereas the active phase and second stage of labor were similar between groups.
Conclusion: Terbutaline use during labor was not associated with a statistically significant higher risk of CD due to labor dystocia among patients undergoing term IOL.
Keywords: Labor management; Terbutaline; Labor dystocia; Fetal distress; Induction of labor; Arrest of labor; Cesarean delivery rate; Cesarean delivery
| Introduction | ▴Top |
Induction of labor (IOL) rates have substantially increased over the past 30 years, with a further increase after publication of the ARRIVE trial in 2018. As of 2021, at least 32% of livebirths in the United States (US) were the result of IOL [1-4]. With IOL on the rise, it is important to understand the best practices for labor management for those undergoing IOL [5].
Terbutaline, a β2-adrenergic agonist, is a commonly used obstetric medication that inhibits uterine tachysystole or tetanic contractions by reducing myometrial activity [6-8]. Though not approved by the US Food and Drug Administration (FDA) as a tocolytic, experts agree that off-label use is appropriate when used for short-term, acute care in the inpatient setting in the appropriate clinical context, most commonly, fetal heart rate changes secondary to uterine tachysystole or tetanic contraction [9].
Studies demonstrate that terbutaline use is associated with improvement in fetal heart rate tracings, increased umbilical artery pH values, higher Apgar scores, and lower neonatal intensive care unit admission rates [10-12]. Most studies on intrapartum terbutaline use focus on its role as an acute tocolytic given prior to cesarean delivery (CD) [10-12]. One meta-analysis showed that beta-agonist use like terbutaline was associated with lower risk of CD for non-reassuring fetal status [11]. For maternal outcomes, studies show that terbutaline is well tolerated with no difference in blood loss at time of CD, and is associated with tachycardia as its most common adverse effects [13, 14].
As a potent inhibitor of uterine myometrial activity known for disrupting uterine contractions, there is biologic plausibility that terbutaline use in labor may negatively impact labor progression and increase risk of labor dystocia. However, limited evidence exists evaluating the potential impact of terbutaline use on risk of CD due to labor dystocia.
Therefore, we sought to assess the association between intrapartum terbutaline administration and CD for labor dystocia in patients undergoing term IOL.
| Materials and Methods | ▴Top |
This was a secondary analysis of a prospective cohort study of patients at an urban academic hospital undergoing IOL from 2013 to 2015 [15, 16]. Study participants were at least 18 years of age, with a full term (≥ 37 weeks) singleton gestation in cephalic presentation with intact membranes, and Bishop score of ≤ 6 and dilation ≤ 2 cm undergoing IOL for any indication. Patients who had a history of CD, a contraindication to vaginal delivery, did not speak English, or had human immunodeficiency virus (HIV), hemolysis, elevated liver enzymes, and low platelets (HELLP) syndrome, eclampsia, or severe intrauterine growth restriction with abnormal umbilical artery Dopplers were excluded. All patients from the parent study were included in this secondary analysis with no post hoc exclusions.
The primary outcome was CD due to labor dystocia, defined as failed IOL, arrest of dilation, or arrest of descent, as documented in the electronic medical record for each patient. All cesarean deliveries that included labor dystocia either in isolation or in combination with other diagnoses as an indication for cesarean were counted as “labor dystocia” for the purpose of our analysis. Comparison groups were those who received ≥ 1 dose of terbutaline versus those who did not receive any intrapartum terbutaline.
Secondary outcomes included length of labor, pre-specified composite maternal morbidity (occurring up to 4 weeks postpartum, defined as third/fourth degree perineal laceration, blood transfusion, endometritis, wound separation/infection, venous thromboembolism, hysterectomy, intensive care unit admission, or death) and pre-specified composite neonatal morbidity (occurring prior to discharge, defined as severe respiratory distress, culture proven/presumed neonatal sepsis, neonatal blood transfusion, hypoxic ischemic encephalopathy, intraventricular hemorrhage grade 3 or 4, necrotizing enterocolitis, or need for head cooling). Generalized linear models were used to calculate relative risk and adjust for potential confounding variables, using forward selection to assess any variables with P < 0.20 in bivariate analysis. A post hoc power calculation was performed: based on our sample size, we had 80% power to detect a 10% difference in our primary outcome between groups. This study was reviewed and approved by the Institutional Review Board of the study site.
| Results | ▴Top |
A total of 844 patients met inclusion criteria: 161 (19%) received terbutaline and 683 (81%) did not (Table 1). As shown in Table 1, the exposed and unexposed groups were similar; there was a significant difference in starting cervical exam dilation (1.0 cm (1.0, 1.50) vs. 1.0 cm (0.5, 1.5), P < 0.01).
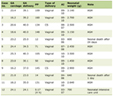 Click to view | Table 1. Baseline Characteristics |
Delivery outcomes can be seen in Table 2. Overall, 51% of patients in the terbutaline group underwent CD, versus 24% in the unexposed group (P ≤ 0.001). This difference was driven by CD for non-reassuring fetal heart rate tracing (NRFHT) (26% exposed vs. 4% unexposed, P < 0.001). The primary outcome, the rate of CD for labor dystocia, was not significantly different between groups (24.8% exposed vs. 19.5% unexposed, P = 0.13), even after adjusting for parity, body mass index (BMI), and initial cervical dilation (adjusted risk ratio (aRR) 1.03 (0.75 - 1.42)). The total median length of labor, defined as time from initiation of induction to delivery of the neonate regardless of ultimate mode of delivery, was approximately two hours longer longer in the terbutaline group (18.3 h (14.1 - 25.8) exposed vs. 16.2 h (10.8 - 23.2) unexposed, P < 0.01).
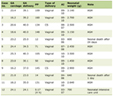 Click to view | Table 2. Delivery Outcomes |
To assess for a possible dose response, we assessed the primary outcome among patients receiving one, two, or more doses of terbutaline, and found no significant differences in CD for dystocia (P = 0.31). Among patients who received one dose of intrapartum terbutaline, 22.3% (n = 21) underwent cesarean for dystocia. For those who received two doses, the rate of CD for dystocia was 26.5% (n = 13) and for those who received three or more doses the rate was 33.3% (n = 6).
There were no statistically significant differences in composite maternal morbidity (8.6% exposed vs. 9.2% unexposed, P = 0.81) or neonatal morbidity (3.1% vs. 2.2%, P = 0.49) between groups.
| Discussion | ▴Top |
This secondary analysis of a prospective cohort study of term patients undergoing IOL found no statistically significant difference in the rate of CD due to labor dystocia among those who received intrapartum terbutaline compared to those who did not. We also found no evidence of a dose-response effect or any increased maternal or neonatal morbidity associated with terbutaline use, though our power to detect these differences was limited by a fixed sample size and this secondary outcome was strictly exploratory.
As expected, the overall rate of CD was higher in the group who received terbutaline during labor; however, this difference was driven by indication, specifically, for fetal intolerance of labor.
While we found a statistically significant two-hour difference in the length of the overall labor course for patients who received terbutaline, this difference is not likely clinically meaningful. However, the additional two hours from induction-to-delivery time may have operational and patient-centered relevance that should be considered.
One of the most compelling strengths of this study is the analysis is based on a clinical prospective cohort study on IOL outcomes. Data derived from prospective clinical studies are limited in obstetrics and analyses that derive from such studies are some of the strongest tools and sources of evidence we have to guide obstetric care. Our study design also used strict definitions for our exposure (whether or not a medication is received) and for outcome (the prospectively collected data on indication for CD).
This study makes an important contribution to the literature, as there is limited available evidence assessing the impact of terbutaline administration on labor dystocia or arrest. While a prior meta-analysis showed decreases in CD for non-reassuring fetal status with terbutaline use, that study did not assess for CD for labor dystocia [11]. Given the rise in IOL, studying the effect of common labor interventions in the context of labor induction is of critical importance.
Our study has several limitations. Given that this study is a secondary analysis of a prospective cohort study on IOL practices, our sample size was fixed and we were therefore at risk for type II error. Additionally, the interplay between terbutaline use, NRFHT, and indication for CD is complex. Given that terbutaline is not randomly assigned and is given in response to clinical events such as NRFHT, there is residual confounding that cannot be fully accounted for in adjusted models and thus causality cannot be fully assessed. We also recognize a limitation in generalizability given that this analysis was limited to patients undergoing IOL which is a unique population compared to those in spontaneous labor. In addition, IOL protocols are ever evolving with new practices and protocols being incorporated clinically over the years. Of note, the initial study was conducted in 2013 - 2015, we suspect that the data continue to be reflective of currently labor practices and guidelines given that the induction practices used in this protocol have become used routinely throughout the United States, likely in part from the results of the parent study, and thus we do feel that the induction methods used are reflective of current obstetric standards and practices in the United States today.
This study provides helpful, practical data to address concerns that terbutaline may negatively impact labor progression. There is a paucity of data in the literature regarding the potential effect of terbutaline on the labor curve and risk of arrest of labor, thus this secondary analysis is a useful addition to the literature base.
Conclusion
This secondary analysis of a prospective cohort study of term patients undergoing IOL found no statistically significant difference in the rate of CD due to labor dystocia among those who received intrapartum terbutaline compared to those who did not.
Acknowledgments
None to declare.
Financial Disclosure
None to declare.
Conflict of Interest
None to declare.
Informed Consent
Informed consent was not necessary to conduct this research.
Author Contributions
All listed authors contributed significantly and appropriately to conducting this study and writing this manuscript. Cecilia Leggett: initial concept, literature review, study design, statistical review, manuscript writing and editing; Lisa Levine: study design, statistical review, manuscript writing and editing; Melissa Wong: study design, statistical review, manuscript writing and editing; Jennifer McCoy: study design, statistical analysis, manuscript writing and editing.
Data Availability
The data supporting the findings of this study are available from the corresponding author upon reasonable request.
Abbreviations
aRR: adjusted risk ratio; BMI: body mass index; CD: cesarean delivery; FDA: Food and Drug Administration; IOL: induction of labor; NRFHT: non-reassuring fetal heart rate tracing; US: United States
| References | ▴Top |
- Grobman WA. The ARRIVE trial. Clin Obstet Gynecol. 2024;67(2):374-380.
doi pubmed - Wood R, Freret TS, Clapp M, Little S. Rates of induction of labor at 39 weeks and cesarean delivery following publication of the ARRIVE trial. JAMA Netw Open. 2023;6(8):e2328274.
doi pubmed - Osterman MJK, Hamilton BE, Martin JA, Driscoll AK, Valenzuela CP. Births: final data for 2021. Natl Vital Stat Rep. 2023;72(1):1-53.
pubmed - Grobman WA, Rice MM, Reddy UM, Tita ATN, Silver RM, Mallett G, Hill K, et al. Labor Induction versus Expectant Management in Low-Risk Nulliparous Women. N Engl J Med. 2018;379(6):513-523.
doi pubmed - Reddy UM, Sandoval GJ, Tita ATN, Silver RM, Mallett G, Hill K, El-Sayed YY, et al. Oxytocin regimen used for induction of labor and pregnancy outcomes. Am J Obstet Gynecol MFM. 2024;6(12):101508.
doi pubmed - Egarter CH, Husslein PW, Rayburn WF. Uterine hyperstimulation after low-dose prostaglandin E2 therapy: tocolytic treatment in 181 cases. Am J Obstet Gynecol. 1990;163(3):794-796.
doi pubmed - Mayer C, Apodaca-Ramos I. Tocolysis. In: StatPearls. Treasure Island (FL) ineligible companies. 2025.
pubmed - Stewart RD, Bleich AT, Lo JY, Alexander JM, McIntire DD, Leveno KJ. Defining uterine tachysystole: how much is too much? Am J Obstet Gynecol. 2012;207(4):290.e291-296.
doi pubmed - ACOG Practice Bulletin. ACOG practice bulletin. Management of preterm labor. Number 43, May 2003. Int J Gynaecol Obstet. 2003;82(1):127-135.
doi pubmed - Tejani NA, Verma UL, Chatterjee S, Mittelmann S. Terbutaline in the management of acute intrapartum fetal acidosis. J Reprod Med. 1983;28(12):857-861.
pubmed - Xodo S, de Heus R, Berghella V, Londero AP. Acute tocolysis for intrapartum nonreassuring fetal status: how often does it prevent cesarean delivery? A systematic review and meta-analysis of randomized controlled trials. Am J Obstet Gynecol MFM. 2022;4(5):100639.
doi pubmed - Zahar AZ, Azny MY, Sakinah A, Gayathiri M. Terbutaline for acute tocolysis prior to emergency caesarean delivery for suspected foetal compromise. Med J Malaysia. 2023;78(1):93-97.
pubmed - Buckley VA, Wu J, De Vries B. Outcomes following acute tocolysis prior to emergency caesarean section. Aust N Z J Obstet Gynaecol. 2020;60(6):884-889.
doi pubmed - Magann EF, Norman PF, Bass JD, Chauhan SP, Martin JN, Jr., Morrison JC. Acute tocolysis for suspected intrapartum fetal distress: maternal effects of terbutaline versus magnesium sulfate. Int J Obstet Anesth. 1995;4(3):140-144.
doi pubmed - McCoy J, Downes KL, Srinivas SK, Levine LD. Postdates induction with an unfavorable cervix and risk of cesarean(). J Matern Fetal Neonatal Med. 2019;32(17):2874-2878.
doi pubmed - Levine LD, Downes KL, Elovitz MA, Parry S, Sammel MD, Srinivas SK. Mechanical and pharmacologic methods of labor induction: a randomized controlled trial. Obstet Gynecol. 2016;128(6):1357-1364.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Gynecology and Obstetrics is published by Elmer Press Inc.