| Journal of Clinical Gynecology and Obstetrics, ISSN 1927-1271 print, 1927-128X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Gynecol Obstet and Elmer Press Inc |
| Journal website https://jcgo.elmerpub.com |
Original Article
Volume 000, Number 000, May 2025, pages 000-000
A Parity-Based Analysis of Women of Advanced Maternal Age and Delivery
Kimitoshi Imai
Imai OB/GYN Clinic, Shizuoka 420-0867, Japan
Manuscript submitted March 6, 2025, accepted May 1, 2025, published online May 8, 2025
Short title: Advanced Maternal Age and Childbirth
doi: https://doi.org/10.14740/jcgo1515
| Abstract | ▴Top |
Background: An increasing number of older mothers are a worldwide concern in obstetrical practice. First labor and delivery is quite different from the second one onward. Therefore, this study aimed to examine the differences in labor and delivery features between nulliparous and multiparous women of advanced maternal age (AMA) and their younger counterparts.
Methods: Women who delivered at our clinic between January 2004 and December 2022 were enrolled. The inclusion criteria were term (≥ 37 weeks), cephalic presentation, and singleton. We excluded women with fetal demise before labor onset, those with uncontrolled medical diseases such as hypertension, hyperthyroidism, diabetes mellitus, and those with scarred uteri. Nulliparous and multiparous women aged ≥ 35 years at delivery were regarded as having AMA, and were compared with women in their twenties as younger counterparts.
Results: In this study, 514 nulliparous and 1,116 multiparous women of AMA, and their younger counterparts (1,432 nulliparous and 845 multiparous women) were enrolled. Of the nulliparous women of AMA, pregnancy by assisted reproductive technology (ART) (13.4% vs. 0.8%, P < 0.001), labor induction (27.2% vs. 12.8%, P < 0.001), prolonged second stage of labor (27.7% vs. 14.8%, P < 0.001), cesarean section (7.2% vs. 1.1%, P < 0.001), and vacuum extraction (16.0% vs. 9.4%, P < 0.001) were significantly more frequent compared to their younger counterparts. Similarly, multiparous women of AMA showed a higher frequency or pregnancies by ART (5.7% vs. 0.1%, P < 0.001), labor induction (19.2% vs. 12.5%, P < 0.001), prolonged second stage of labor (5.2% vs. 2.1%, P < 0.001), and vacuum extraction (4.3% vs. 1.5%, P < 0.001) compared to their younger counterparts. However, cesarean section rates (0.2% vs. 0.0%, P = 0.22) were similar.
Conclusions: Pregnant women of AMA had different clinical risks due to parity. However, a vast majority had successful vaginal deliveries.
Keywords: Advanced maternal age; Labor and delivery; Duration of labor; Mode of delivery; Parity
| Introduction | ▴Top |
The increasing rate of cesarean sections (CS) is a global issue in obstetrical practice [1-3]. The higher rate of CS is due to the increasing number of older mothers. In many developed countries, it is common for young couples to delay marriage and pregnancy. In the United States, the age of mothers at first childbirth rose from 21.4 in 1970 to 24.9 in 2000, reaching 26.3 in 2014 and 27.4 in 2022 [4-6]. In Japan, the age at first childbirth increased from 25.7 in 1975 to 30.7 in 2019 [7]. In many European countries, mothers aged ≥ 35 years account for 20% of all births, and over 30% in Spain and Ireland in 2019 [8].
Advanced maternal age (AMA) is one of the dystocia-related factors in nulliparous women [9], and it is responsible for many detrimental effects on pregnancy, such as stillbirth, miscarriage, preterm labor, gestational diabetes mellitus, hypertensive disorders of pregnancy, and preeclampsia [10-12]. Reportedly, AMA is associated with higher CS rates in nulliparous and multiparous women [13-15]. However, we reported a very low primary CS rate in low-risk multiparous women [16]. Therefore, in this study, we aimed to examine the clinical differences in labor and delivery between nulliparous and multiparous women of AMA and their younger counterparts.
| Materials and Methods | ▴Top |
In this study, we enrolled women who delivered between January 2004 and December 2022 at our clinic in Shizuoka City, a central Japanese city with approximately 700,000 inhabitants. The inclusion criteria were: cephalic presentation, singleton, and term pregnancy (≥ 37 weeks gestation). We excluded women with fetal demise before labor onset, those with uncontrolled medical diseases such as hypertension, hyperthyroidism, and diabetes mellitus and women with scarred uteri. Women of AMA (≥ 35 years at delivery) and their younger counterparts in their twenties were analyzed for parity (only for multiparous women), maternal height, maternal prepregnancy body weight, prepregnancy body mass index (BMI), gestational age, gestational weight gain (GWG), neonatal weight, neonatal head circumference, amount of blood loss, pregnancy by assisted reproductive technology (ART), umbilical artery (UA) pH, UA base excess, Apgar score at 5 min ≤ 7, labor induction, use or non-use of epidural analgesia, duration of first and second stage of labor, and mode of delivery. Nulliparous and multiparous women were analyzed separately. Notably, forceps delivery was not performed in our clinic.
The local Ethics Committee approved this study (approval no. 23007). SPSS for Windows (version 22.0; IBM, Tokyo, Japan) was used for the statistical analysis. A value < 0.05 was considered as statistically significant.
| Results | ▴Top |
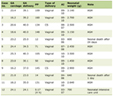
We enrolled 514 nulliparous and 1,116 multiparous women of AMA, along with 1,432 nulliparous and 845 multiparous women as younger counterparts. Table 1 presents their demographic and clinical characteristics. The mode of delivery, indication for CS, duration of labor, and frequency of prolonged labor are presented in Tables 2-5, respectively.
 Click to view | Table 1. Demographic and Clinical Characteristics of Women of AMA and Their Younger Counterparts (in Their Twenties) |
 Click to view | Table 2. Mode of Delivery |
 Click to view | Table 3. Indication for Cesarean Sections |
 Click to view | Table 4. Duration of Labor |
 Click to view | Table 5. Frequency of Prolonged Labor |
Compared to their younger counterparts, the nulliparous and multiparous women of AMA exhibited significantly heavier body weight and BMI, lower GWG, higher rate of pregnancy by ART, labor induction, and use of epidurals (Table 1).
Regarding mode of delivery, nulliparous women of AMA had a higher rate of vacuum extraction (16.0% vs. 9.4%, P < 0.001) and CS (7.2% vs. 1.1%, P < 0.001), compared to their younger counterparts. In contrast, multiparous women of AMA had a higher rate of vacuum extraction (4.3% vs. 1.5%, P < 0.001) compared with their younger counterparts. However, they had similar CS rates (0.2% vs. 0.0%, P = 0.218) (Table 2). The indication for CS was mainly cephalopelvic disproportion/failure to progress among nulliparous women of AMA and their younger counterparts (Table 3). We enrolled only low-risk pregnant women; hence, no CS was performed before the onset of labor.
Nulliparous (median, 527 vs. 570 min, P = 0.16) and multiparous (median, 245 vs. 265 min, P = 0.052) women of AMA and their younger counterparts had similar duration of first stage of labor. However, when epidural users were excluded, the duration of first stage of labor in multiparous women of AMA was significantly shorter than that of their younger counterparts (median 245 vs. 265 min, P = 0.035) (Table 4).
Nulliparous and multiparous women of AMA had a significantly longer duration of second stage of labor than their younger counterparts (nulliparous: median 77 vs. 50 min, P < 0.001; multiparous: median 14 vs. 11 min, P < 0.001) (Table 4). When epidural users were excluded, the duration of second stage of labor was also significantly longer in nulliparous and multiparous women of AMA than in their younger counterparts (Table 4).
Threshold comparisons showed that AMA group had a similar frequency of prolonged first stage of labor (> 20 h for nulliparous women and > 14 h for multiparous women) with younger counterparts in both nulliparous (12.2% vs. 13.6%, P = 0.48) and multiparous women (3.0% vs. 2.6%, P = 0.68). However, the frequency of prolonged second stage of labor (> 2 h and > 1 h for nulliparous and multiparous women, respectively; with 1 h added for epidural analgesia) was higher in women of AMA than in their younger counterparts in both nulliparous (27.7% vs. 14.8%, P < 0.001) and multiparous (5.2% vs. 2.1%, P < 0.001) women (Table 5).
| Discussion | ▴Top |
Many studies have shown that pregnancy in AMA is associated with adverse outcomes for both mother and baby [10-15]. In this study, we enrolled only women with low-risk pregnancies and aimed to clarify whether “healthy” AMA affected the mode of delivery and duration of labor irrespective of parity. As progress of labor and CS rate among nulliparous and multiparous women are quite different [17, 18], it is reasonable to analyze them separately. It has been shown in many studies that AMA is associated with longer labor durations and higher rates of instrumental delivery and CS [13-15]. However, the relationship between maternal age and labor duration is complex. Greenberg et al reported that the duration of labor and prolonged labor increased with increasing maternal age [19]. However, in their study, the duration of first stage of labor did not differ between young (< 20 years) and older women (20 to above 40 years) without epidural use in either the nulliparous or multiparous groups. The duration of second stage of labor differed between young and older women in the nulliparous and multiparous groups irrespective of epidural use. Zaki et al also reported that first stage of labor progressed more quickly with increasing age among nulliparous women up to 40 years old, and all multiparous women. In contrast, the duration of the second stage of labor increased along with increased maternal age [20].
Wang et al reported that among nulliparous women, AMA was associated with a higher frequency of CS before labor (odds ratio (OR): 2.26, P < 0.005) and in labor (OR: 1.44, P = 0.016), and more instrumental deliveries (OR: 1.49, P = 0.004) compared with their younger counterparts [21]. However, they reported similar CS rate in labor (OR: 1.22, P = 0.168), and instrumental delivery (OR: 1.35, P = 0.058) in multiparous women of AMA compared with younger multiparous women. Crequit et al also showed that among nulliparous women at term in spontaneous labor, AMA was not associated with an increased intrapartum CS rate [22]. Consistent with these previous studies, we suggest that women of AMA are not always associated with longer labor or more difficult labor.
Declined uterine contractility [23], decreased maternal physical strength [24, 25], and the obstetricians’ lower threshold for performing CS in women of AMA [14, 26] could be the reasons why pregnant women of AMA have longer labor and more frequent dystocia-related CS than their younger counterparts. Until recently, uterine contractility was believed to not decline with aging [27, 28]. However, Punson-Jimenez et al showed that uterine contractility declines with aging [23]. Elmenshawy et al [24] and Chomik and Jacinto [25] reported that female physical performance peaks in their twenties for many sports. These findings may explain the longer duration of labor and more frequent dystocia-related CS in women of AMA. Rydahl et al suggested that obstetrical culture such as early intervention and a higher induction rate for women of AMA may contribute to a higher rate of dystocia-related CS [14]. Zeevi et al postulated that a higher rate of CS in the older group might be due to physician’s inclination to opt more easily for CS during labor [26].
Is there an age limit for vaginal delivery [26]? The author has never thought that women could be too old for vaginal delivery. However, if nulliparous women in their late 40s or 50s had visited our clinic for delivery, my opinion may change.
This study had several limitations. First, in both nulliparous and multiparous groups of AMA, the oldest women were 45 years old (Table 1). If a significant number of mothers of AMA (≥ 45 years old) were included, our results would be different [29]. Second, in our clinic, epidural analgesia was used in < 10% of our cases (Table 1). In Japan, epidural use during labor has been low [30]. In 2016, only 6.1% of women used epidural analgesia during labor [30]. If epidural analgesia had been used more frequently, the duration of labor and mode of delivery may have been different. Third, this study was done in a single clinic, which may limit generalizability of the findings.
This study had several strengths. The decision to perform CS was made by a single physician, reducing variability. As CS rate is quite different among doctors and hospitals [31, 32], its indication may be quite subjective [33]. Hence, inter-hospital and inter-physician biases were avoided in this study. Second, a longer time was allowed for first and second stages of labor (Table 3). If CS had been performed quickly for cases with a slightly longer duration of labor, there might have been no difference in the duration of labor between women of AMA and their younger counterparts.
Furthermore, many women of AMA are anxious about their childbirth, and anxiety and fear of childbirth may cause dystocia [34]. This study’s findings may relieve their fear of labor and delivery as the vast majority of women had successful vaginal births.
Conclusions
In nulliparous and multiparous women, the duration of second stage of labor was longer in those of AMA than in their younger counterparts. However, that of first stage was not. Multiparous women of AMA had similar CS rate, whereas nulliparous women of AMA had higher CS rate than their younger counterparts. Women of AMA are not homogenous, and their risks should be considered individually.
Acknowledgments
The author is grateful to the coworkers of this clinic including nurses and midwives, for their professional efforts and devotion to labor and delivery.
Financial Disclosure
This research did not receive any grants or financial support.
Conflict of Interest
None to declare.
Informed Consent
Not applicable.
Author Contributions
KI performed all the research including research design, data collection and analysis, and manuscript writing.
Data Availability
The data of this study are available from the corresponding author upon reasonable request.
Abbreviations
AMA: advanced maternal age; ART: assisted reproductive technology; BMI: body mass index; CPD: cephalopelvic disproportion; CS: cesarean section; FTP: failure to progress; GWG: gestational weight gain; NRFS: non-reassuring fetal status; OR: odds ratio; UA: umbilical artery
| References | ▴Top |
- World Health Organization. Caesarean section rates continue to rise, amid growing inequalities in access. Rising rates suggest increasing numbers of medically unnecessary, potentially harmful procedures. 2021.
- Betran AP, Ye J, Moller AB, Souza JP, Zhang J. Trends and projections of caesarean section rates: global and regional estimates. BMJ Glob Health. 2021;6(6):e005671.
doi pubmed - The L. Stemming the global caesarean section epidemic. Lancet. 2018;392(10155):1279.
doi pubmed - Mathews TJ, Hamilton BE. Mean age of mother, 1970-2000. Natl Vital Stat Rep. 2002;51(1):1-13.
pubmed - Mathews TJ, Hamilton BE. Mean age of mothers is on the rise: United States, 2000-2014. NCHS Data Brief. 2016;232:1-8.
pubmed - Osterman MJK, Hamilton BE, Martin JA, Driscoll AK, Valenzuela CP. Births: final data for 2022. Natl Vital Stat Rep. 2024;73(2):1-56.
pubmed - Ministry of Health, Labour and Welfare. Vital statistics of Japan 2019. 2022.
- Euro-Peristat. European perinatal health report, 2015-2019. Core indicators of the health and care of pregnant women and babies in Europe from 2015 to 2019.
- Imai K. A retrospective observational study on the predisposing factors for dystocia-related cesarean section among low-risk term nulliparous women. Eur Gynecol Obstet. 2023;5(1):34-38.
doi - Frick AP. Advanced maternal age and adverse pregnancy outcomes. Best Pract Res Clin Obstet Gynaecol. 2021;70:92-100.
doi pubmed - Glick I, Kadish E, Rottenstreich M. Management of pregnancy in women of advanced maternal age: improving outcomes for mother and baby. Int J Womens Health. 2021;13:751-759.
doi pubmed - Cavazos-Rehg PA, Krauss MJ, Spitznagel EL, Bommarito K, Madden T, Olsen MA, Subramaniam H, et al. Maternal age and risk of labor and delivery complications. Matern Child Health J. 2015;19(6):1202-1211.
doi pubmed - Waldenstrom U, Ekeus C. Risk of labor dystocia increases with maternal age irrespective of parity: a population-based register study. Acta Obstet Gynecol Scand. 2017;96(9):1063-1069.
doi pubmed - Rydahl E, Declercq E, Juhl M, Maimburg RD. Cesarean section on a rise-Does advanced maternal age explain the increase? A population register-based study. PLoS One. 2019;14(1):e0210655.
doi pubmed - Xie M, Lao TT, Du M, Sun Q, Qu Z, Ma J, Song X, et al. Risk for Cesarean section in women of advanced maternal age under the changed reproductive policy in China: A cohort study in a tertiary hospital in southwestern China. J Obstet Gynaecol Res. 2019;45(9):1866-1875.
doi pubmed - Imai K. Primary cesarean section in term, low-risk multiparous women: a single clinic retrospective observational study. Obstet Gynecol Int J. 2021;12(1):10-13.
doi - Zhang J, Landy HJ, Ware Branch D, Burkman R, Haberman S, Gregory KD, Hatjis CG, et al. Contemporary patterns of spontaneous labor with normal neonatal outcomes. Obstet Gynecol. 2010;116(6):1281-1287.
doi pubmed - El Radaf V, Campos LN, Savona-Ventura C, Mahmood T, Zaigham M. Robson ten group classification system for Caesarean sections across Europe: A systematic review and meta-analysis. Eur J Obstet Gynecol Reprod Biol. 2025;305:178-198.
doi pubmed - Greenberg MB, Cheng YW, Sullivan M, Norton ME, Hopkins LM, Caughey AB. Does length of labor vary by maternal age? Am J Obstet Gynecol. 2007;197(4):428.e421-427.
doi pubmed - Zaki MN, Hibbard JU, Kominiarek MA. Contemporary labor patterns and maternal age. Obstet Gynecol. 2013;122(5):1018-1024.
doi pubmed - Wang Y, Tanbo T, Abyholm T, Henriksen T. The impact of advanced maternal age and parity on obstetric and perinatal outcomes in singleton gestations. Arch Gynecol Obstet. 2011;284(1):31-37.
doi pubmed - Crequit S, Korb D, Schmitz T, Morin C, Sibony O. Impact of maternal age on intrapartum caesarean delivery rate in nulliparas with spontaneous labour. J Gynecol Obstet Hum Reprod. 2019;48(6):407-411.
doi pubmed - Punzon-Jimenez P, Machado-Lopez A, Perez-Moraga R, Llera-Oyola J, Grases D, Galvez-Viedma M, Sibai M, et al. Effect of aging on the human myometrium at single-cell resolution. Nat Commun. 2024;15(1):945.
doi pubmed - Elmenshawy AR, Machin DR, Tanaka H. A rise in peak performance age in female athletes. Age (Dordr). 2015;37(3):9795.
doi pubmed - Chomik R, Jacinto M. Peak performance age in sport. 2021. Cepar, Arc Centre of Excellence in population ageing research. www.cepar.edu.au.
- Zeevi G, Zlatkin R, Hochberg A, Danieli-Gruber S, Houri O, Hadar E, Walfisch A, et al. Is there an age limit for a trial of vaginal delivery in nulliparous women? J Clin Med. 2023;12(11):3620.
doi pubmed - Arrowsmith S, Robinson H, Noble K, Wray S. What do we know about what happens to myometrial function as women age? J Muscle Res Cell Motil. 2012;33(3-4):209-217.
doi pubmed - Crankshaw DJ, O'Brien YM, Crosby DA, Morrison JJ. Maternal age and contractility of human myometrium in pregnancy. Reprod Sci. 2015;22(10):1229-1235.
doi pubmed - Ogawa K, Urayama KY, Tanigaki S, Sago H, Sato S, Saito S, Morisaki N. Association between very advanced maternal age and adverse pregnancy outcomes: a cross sectional Japanese study. BMC Pregnancy Childbirth. 2017;17(1):349.
doi pubmed - Maeda Y, Takahashi K, Yamamoto K, Tanimoto T, Kami M, Crump A. Factors affecting the provision of analgesia during childbirth, Japan. Bull World Health Organ. 2019;97(9):631-636.
doi pubmed - Metz TD, Allshouse AA, Gilbert SAB, Doyle R, Tong A, Carey JC. Variation in primary cesarean delivery rates by individual physician within a single-hospital laborist model. Am J Obstet Gynecol. 2016;214(4):531.e1-e6.
doi pubmed - Riddell CA, Hutcheon JA, Strumpf EC, Abenhaim HA, Kaufman JS. Inter-institutional variation in use of caesarean delivery for labour dystocia. J Obstet Gynaecol Can. 2017;39(11):988-995.
doi pubmed - Tita AT. When is primary cesarean appropriate: maternal and obstetrical indications. Semin Perinatol. 2012;36(5):324-327.
doi pubmed - Laursen M, Johansen C, Hedegaard M. Fear of childbirth and risk for birth complications in nulliparous women in the Danish National Birth Cohort. BJOG. 2009;116(10):1350-1355.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Gynecology and Obstetrics is published by Elmer Press Inc.